Measurement-Based Care in Child and Youth Mental Health
- The Impact of Measurement-Based Care
- What is Measurement-Based Care?
- MBC helps Providers and Organizations Gain Perspective
- MBC and Therapeutic Alliance
- Demonstrate Value With MBC
- Tips for Implementing Measurement-Based Care with Children & Youth
- The Value of Technology: Integrating Data Across the System
- Promote a Culture of Learning and Engagement
- Deliver Personalized Care with MBC
In our recent webinar, Advancing Child & Youth Mental Health with Measurement-Based Care, leaders from across the field came together to share how they are using Measurement-Based Care (MBC) to transform services for children, youth, and families. The discussion highlighted the importance of MBC, and how systemic measurement can help organizations provide better care, support more meaningful engagement, and demonstrate impact to everyone involved, from young people and their caregivers, to clinicians, funders, and stakeholders.
This article revisits some of the powerful insights from the session, featuring clips from our panelists from CARF, the National Council for Mental Wellbeing, and UConn Health, to provide a comprehensive look at MBC in child and youth mental health settings.
The Impact of Measurement-Based Care
What is Measurement-Based Care?
Measurement-Based Care is the routine collection of patient-reported outcome measures to monitor symptoms and progress over time, and using that data to inform collaborative discussions and treatment plans. Our panelists emphasized that MBC is not about replacing clinical judgment; instead, it’s about augmenting it with consistent, objective data throughout care.
By regularly using validated assessment tools to track symptoms with MBC, clinicians can:
- Gain a more accurate and comprehensive picture of a clients’ experience
- Make data-informed clinical decisions
- Meaningfully engage clients in discussions and throughout treatment
- Demonstrate program effectiveness to funders and stakeholders.
MBC helps Providers and Organizations Gain Perspective
One of the most compelling benefits of MBC is its ability to help clinicians and teams “zoom out” and see macro patterns they might otherwise miss in the day-to-day flow of sessions. Instead of relying solely on clinical impressions, MBC provides structured data over time to create a broader lens on the client’s experience.
In the clip below, Dr. David FitzGerald, Assistant Professor, Department of Psychiatry, and Director, Child & Adolescent Psychiatry Outpatient Clinic at UConn Health, explains how longitudinal data helps both clinicians and youth see the bigger picture of their progress, and how that perspective can empower young people by giving them autonomy over their own care.
This broader perspective is not only useful in clinical settings, it also helps leaders reflect on program and organization-level effectiveness, identifying strengths, and targeting areas for improvement. Dr. Jeff Capobianco, Senior Consultant at the National Council for Mental Wellbeing, spoke about how, in child and youth settings in particular, they’ve seen tremendous value in “data telling a story,” where MBC offers perspective on their services and helps make their clinical work easier and more focused.
Together, these perspectives highlight a core impact of MBC: it turns individual encounters into an ongoing narrative of care, one that can guide decisions at the client, clinician, and system levels.
MBC and Therapeutic Alliance
A common question from clinicians is how standardized assessments and structured measurement might impact the therapeutic relationship, especially with children and teens. Our panelists emphasized that when implemented thoughtfully, MBC can meaningfully enrich the therapeutic alliance by giving young people new ways to express themselves and feel heard throughout care.
Theresa Lindberg, Managing Director for Child and Youth Services at CARF International, offered a powerful story about a youth experiencing anxiety who struggled to put their experience into words during sessions. By leveraging their MBC results and the measures themselves, this young person was able to communicate more clearly and accurately how they were feeling, which opened a new channel of understanding between them and their clinician.
By creating an additional level of communication, MBC can validate a young person’s internal experience, provide concrete starting points for discussion, and help clinicians and youth collaborate on treatment plans and goals, reinforcing a sense of co-ownership and partnership over the direction of care.
Demonstrate Value With MBC
Beyond its clinical impact, MBC plays a crucial role in demonstrating value to stakeholders, including payers, funders, system leaders, and policymakers. As child and youth services move toward more accountable, outcome-focused models, having access to reliable data is essential for telling a clear and compelling story about the quality and impact of care.
This is especially critical in the context of rising rates of mental health challenges among children and young people. Demand for services continues to grow, while funding often remains constrained or fragmented. Consistent, sustained investment in child and youth mental health services depends on the ability to clearly demonstrate need, effectiveness, and impact over time. MBC provides the evidence base required to support continued and increased funding by showing not just service utilization, but measurable improvements in outcomes for young people.
Jeff highlighted how MBC data supports value-based care (VBC) by translating everyday clinical work into measurable outcomes that stakeholders can understand. In the clip below, he describes how organizations are using MBC to demonstrate that the services they deliver are making a meaningful difference and to advocate for the funding necessary to continue innovating and improving the care they provide.
David shares UConn Health’s experience of this, to offer a concrete example of how it can look in practice. Beginning with a pilot in 2023, his team implemented MBC and used the resulting data to demonstrate effectiveness and refine their approach. That evidence base has been critical in building the case for scaling MBC across the organization and investing in it long term.
In the clip below, David explains how collecting and using outcome data enabled his team to clearly demonstrate the effectiveness of their services to institutional stakeholders and decision-makers, enabling the expansion of their MBC implementation from a pilot program to a full rollout.
Tips for Implementing Measurement-Based Care with Children & Youth
The impact of MBC is amplified when it’s woven into the fabric of everyday practice and system operations. Our panelists underscored that implementation is both a technical and a cultural project, requiring the right tools, the right workflows, and a commitment to continuous learning from staff and stakeholders.
The Value of Technology: Integrating Data Across the System
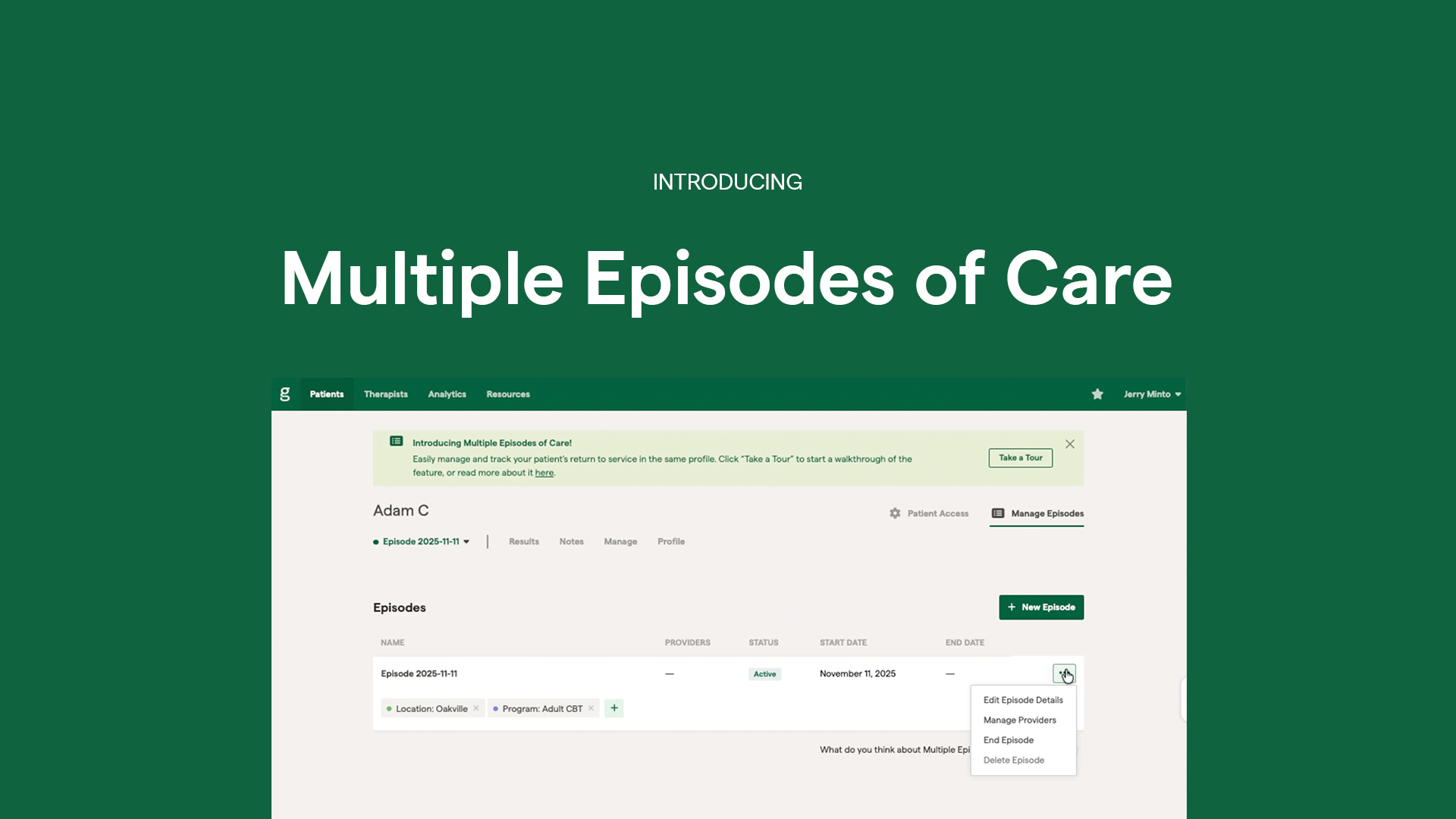
For MBC to be sustainable and scalable, data needs to flow seamlessly from client assessments, to clinician dashboards, to organizational reports and quality improvement initiatives. That’s where purpose-built platforms make a critical difference.
Jeff spoke about how Greenspace supports organizations in choosing and using the right measures, integrating with EHRs/EMRs, and giving clinicians access to resources that empower them to explain MBC to clients in clear, accessible ways. This combination of technical integration and communication support is key to embedding MBC into daily practice.
To further reduce administrative burden and support clinician adoption, the Greenspace platform automates the assessment process and surfaces insights from the data. Jesse Hayman, our Chief Growth Officer, shared how clinicians have found it valuable to have a platform that automatically analyzes scores and trends, and delivers actionable insights they can easily leverage during sessions.
These kinds of integrations and automations support a meaningful, data-informed care journey where assessments are delivered and collected consistently, data is visualized clearly for clinicians and clients, and organizational leaders can access real-time insights into outcomes and engagement.
Promote a Culture of Learning and Engagement
Successfully implementing MBC relies beyond the technology; it requires a culture of learning, where data is embraced as a tool for growth, rather than a mechanism of surveillance or performance.
David emphasized the importance of training future clinicians to use evidence-based decision-making as a core part of their practice. In the clip below, he shares an example using PHQ-9 data to highlight how standardized measures can reveal important information that might be missed if a clinician relied solely on interactions in sessions.
When data is used to support learning, improvement, and advocacy across clinical teams, it becomes a shared asset that benefits clinicians, clients, and the broader mental health system.
Deliver Personalized Care with MBC
While MBC is often associated with standardized tools, our panelists repeatedly underscored its role in driving a personalized care experience. Data empowers clinicians to move beyond one-size-fits-all approaches by:
- Identifying which interventions are working for each client
- Adjusting goals and strategies based on real-time feedback
- Recognizing early signs that a young person may be disengaging or struggling.
The “zoom out” mindset David described, combined with the narrative power of data that Jeff highlighted, creates a foundation for more tailored care journeys. Teens, in particular, benefit when they can see their own graphs and scores, interpret what they mean, and actively participate in decisions about next steps. This reinforces autonomy, agency, and trust, helping clinicians deliver the right support, at the right time, in ways that resonate with the young clients they serve.
Wrapping Up
The insights from the session make it abundantly clear that Measurement-Based Care is no longer optional if, as an industry, we want to advance child and youth mental health in a meaningful, sustainable way.
As Theresa reminded us, “If you don’t measure something, you really can’t improve it.” Through the stories and examples shared by our panelists we can see how organizations are turning this principle into action by using MBC as a powerful tool to drive better care experiences, better outcomes, and a stronger future for the children, youth, and families they serve.
Interested in learning more about MBC for child and youth settings? Schedule a call with an implementation specialist or reach out at info@greenspacehealth.com.