PHQ-9 Three Ways
One of the main components of Measurement-Based Care (MBC) is using assessments and data as a jumping off point for collaboration and discussion between a client and clinician. The process of MBC helps clients better understand and share their own experiences, which empowers them to communicate their thoughts, feelings, behaviours and questions to their clinician. Likewise, clinicians can explore client-reported data to identify symptom changes or patterns, get curious with results to inform their discussions in session and to better understand the experience and needs of their clients. When MBC is looked at as a tool and process to help inform care discussions and decisions, it’s easy to understand how, and why, it helps to improve therapeutic alliance and treatment outcomes.
During our 2nd educational panel with our partners at the Yale Measurement-Based Care Collaborative, we all participated in an important exercise to illustrate how simple, yet valuable, using MBC in care can be.
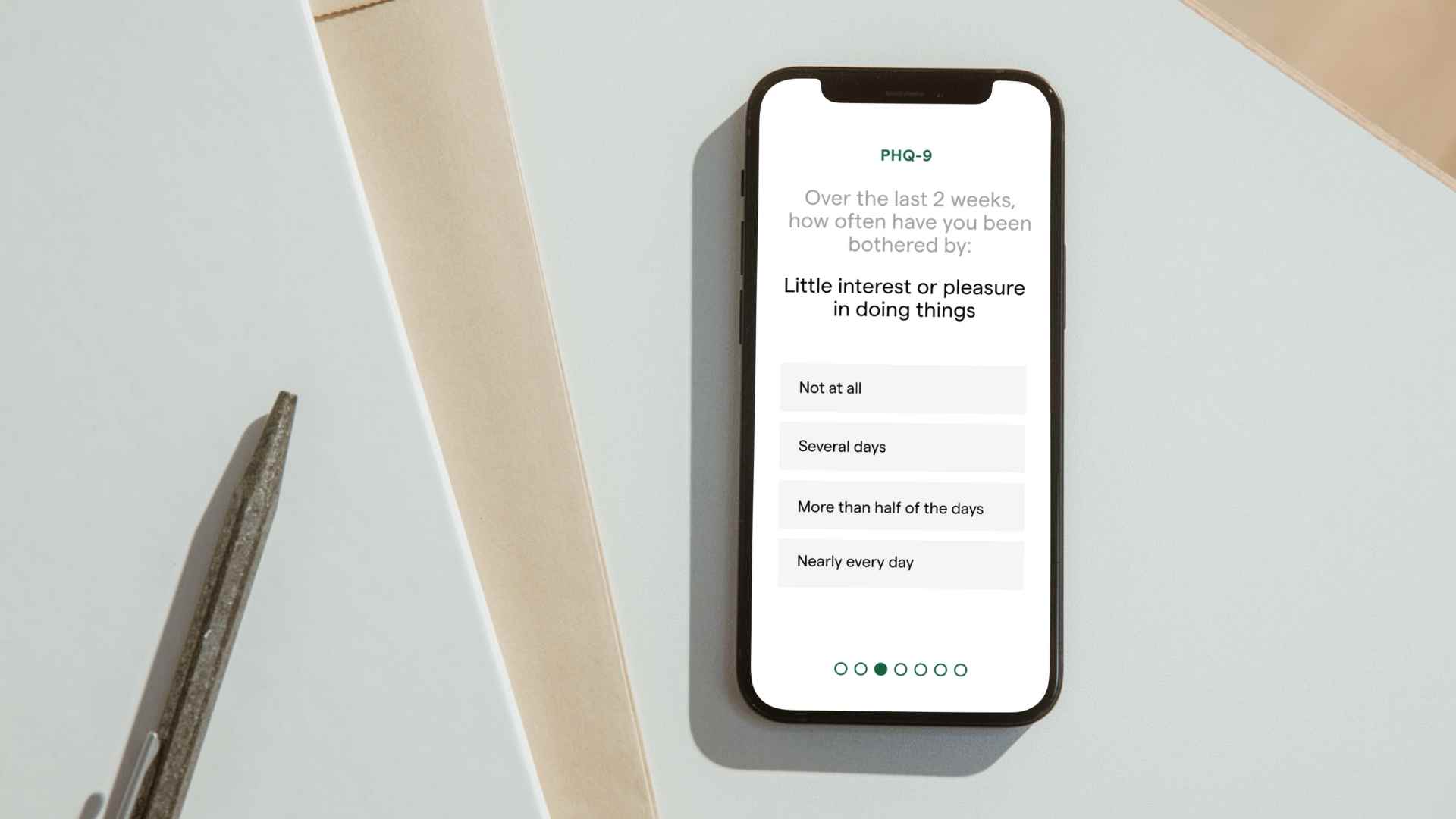
The ‘PHQ-9 Three-Ways’ exercise is used by the team at Yale to help any service provider feel comfortable with the simple process of exploring MBC data and getting curious, alongside their clients, to understand what it may be saying.
How it worked:
The Yale MBC Collaborative shared examples PHQ-9 scores from three different clients—all with slightly different responses. The audience then looked at the responses and shared what they noticed, what hypotheses they were forming, and what they might ask the client in session to dig deeper into their experience.
Watch this clip and try it for for yourself! Then keep reading to learn the key takeaways from the exercise:
Key Learnings
- Data scoring and interpretation is much simpler than it seems. While you might find working through this process in session with a client intimidating, the exercise shows just how easy it is to pick up on what the scores may be telling us. These initial ideas are great to then bring up with your client, to explore the symptoms they’ve reported and have them add context to their responses, through their own thoughts, understanding and experiences.
- Overall assessment(s) scores are helpful, but not as useful as digging into individual items with clients. Two clients could have the same score on a PHQ-9 (or any assessment) but be experiencing completely different symptoms. This is why it’s important to breakdown the scores together and discuss their interpretation of assessment questions and the unique ways symptoms may be presenting for, or impacting, the client.
- It’s about developing a shared language. Personal assessment results give clients a new way to learn about their own mental health, which can help empower them to communicate and participate in ways they may not have been able to otherwise. It can help you and your client have a shared understanding of their experiences and work together throughout the care process.
- Focusing on clinical value first is fundamental. It’s vital to realize that data itself is not the end. It’s the process of exploring data and getting curious that makes MBC so valuable, and helps to engage clients in the process. By treating measurement as a clinical process and incorporating it into sessions with the client, we can discover the clinical value in client-reported data, contributing to a higher therapeutic alliance and improved outcomes for people in care.
- Practice, practice, practice. Practice is the best way to build confidence in the process before trying it out in session. For clinical leaders implementing MBC, consider running your clinics and clinicians through practice sessions using hypothetical client results (like we did in the session above!) . Not only can they work on the “share” process together, but they can even work on how they will initially introduce the process MBC to clients in session. This is one of the best ways to help your clinics and clinicians understand the value of the MBC and how it can positively impact clinical discussions.
- No prep necessarily needed! You don’t have to have answers formed before you draw in your client to talk about it, you can discover them together. An interactive conversation in session can let your client see that you’re making sense of the measure in real time, based on their perspective. It can also be helpful for your process to have the client in the room to fill in any blanks or questions that might arise as you work through the scores. Talk out loud and draw in your client, using your discussion as a way of making the processing of a measure collaborative.