Q&A from ‘Structuring Measurement-Based Care for Success’
In our recent educational webinar with The Lincoln Center and Zócalo Health, Structuring Measurement-Based Care for Success: Implementation Strategies to Drive Adoption, Engagement, and Outcomes, we unpacked what it really takes to successfully implement and sustain Measurement-Based Care (MBC). Our speakers shared how they structured their rollout, supported clinician engagement, aligned MBC with existing workflows, and used outcome data to strengthen care quality.
The conversation sparked a number of insightful questions from attendees, many of which we didn’t have time to address during the live session. We’ve pulled together responses to those unanswered questions, offering practical guidance, real-world lessons, and implementation insights for organizations at every stage of their MBC journey.
Need a refresher before jumping in? Check out the full recording here.
Access, Equity, and Barriers to Care
At Zócalo Health, how did population-level barriers to accessing care (stigma, inequity, logistics, etc.) shape measurement choices or outreach strategies?
At Zócalo Health, the “why” for MBC was rooted in addressing systemic inequities and meeting the needs of their community. More than 60% of Latino adults in community settings are never screened for depression and anxiety, and white adults are screened at nearly double the rate of many minority groups.
To address this, Zócalo:
- Implemented universal screening at all entry points.
- Selected tools (PHQ-9, GAD-7, and PREPARE) that are validated in Spanish, reflecting their primarily monolingual Spanish-speaking population and the social needs profile of the communities they serve.
- Regularly uses aggregate MBC data to identify low utilizers and disengaged members, and re-engage people when follow-up screens show emerging needs.
What is the best way to support older adult clients in using Greenspace?
When integrating technology into care for older adults, the key is to adapt both the technology and workflows to their comfort level, while providing a bit more structure at the start.
Explaining the value of measures, how they will be used to monitor symptoms and guide care, and how results inform clinical discussions can provide important context for clients. From there, depending on their comfort with technology, clinicians may plan for assessment completion during session check-ins, using a kiosk in the waiting area or a tablet in the session room. Staff can also read items aloud and input responses when literacy, vision, or motor issues are a factor.
As clients become more comfortable completing measures, it’s easy to transition to other methods of completion. Assessments in Greenspace are accessible through email, SMS, or clinic kiosks, allowing older adults to complete assessments using the method they’re most comfortable with. With remote delivery, user login is not required, eliminating the need to remember passwords or navigate new software.
How do youth and families access support through Greenspace?
Greenspace can be accessed by clients through their existing clinical provider or program. Clinicians can create profiles for youth and caregivers (or have them automatically created through an EHR integration), assign age-appropriate measures, and review results together in session as part of treatment. Families can also log in through a secure account to view the client’s progress over time, helping everyone stay aligned between visits.
Youth and caregivers may receive assessments by email or SMS to complete on their own device, or they can complete them on a clinic kiosk or tablet with staff support.
Client and Clinician Buy-In, Training, and Long-Term Momentum
How do you onboard new staff into MBC workflows to ensure long-term consistency?
The panelists described two onboarding approaches commonly seen across Greenspace partners:
Zócalo Health treats MBC as part of the clinician’s role, not an optional add-on. New clinicians are trained on how to use Greenspace and interpret data, and expectations around MBC are integrated into quarterly performance reviews. The organization focuses on whether clinicians are logging in, assigning tools, reviewing results, and using dashboards in supervision—rather than holding them accountable for every missed client assessment.
TLC Wellness emphasizes MBC as a clinical tool and support, not a compliance metric. New staff are trained on how measurement supports formulation, treatment planning, and collaboration with schools and community partners. For larger agencies, Emily recommends launching a pilot group and identifying clinician champions who can help colleagues problem-solve and share real-world wins.
In both approaches, sustainable adoption comes from combining clear expectations, high-quality training, and visible clinical value.
What concerns or apprehensions do clinicians and clients raise most often during implementation?
Training and education are critical to successful MBC adoption. Clinicians often ask which assessments to use, how to interpret scores meaningfully, and how to introduce assessments without adding administrative burden. That’s why Greenspace offers a range of features and educational resources to support sustainable, meaningful MBC adoption—reducing workload and allowing clinicians to focus on what matters most: using insights to inform treatment.
- Greenspace integrates with over 85 EHRs to support the seamless adoption of MBC within existing workflows.
- Our Assessments Hub provides detailed guidance on over 40 commonly used assessments, including intended use, administration tips, and interpretation guidance.
- Through our partnership with the Yale MBC Collaborative, we created the Yale MBCC Hub, which includes practical implementation strategies and resources such as how to introduce MBC to clients.
- Our dedicated Customer Success team supports implementation planning, clinician engagement, and long-term adoption.
Clients are typically curious about why assessments matter and how they will be used. Taking time to explain the value of MBC, what the process will look like, and how results will inform sessions encourages participation and engagement.
What have you found to be the most effective way to get patients to complete assessments?
The most effective strategy is clearly connecting assessments to client goals and consistently using results in treatment conversations. Early on, clinicians should explain why measures are used, how they support care, and how clients can view their progress. When clients can see changes visually and discuss them in session, MBC becomes a meaningful part of care.
Greenspace supports automated SMS or email delivery, with reminders sent after 24–48 hours to encourage completion at a convenient time.
Watch the following video, where Jessica Barber from the Yale MBC Collaborative shares tips on introducing MBC to clients and fostering engagement:
How do organizations maintain momentum with MBC over time?
Momentum is sustained when MBC is treated as part of everyday care rather than a time-limited project. Regularly assigning assessments, reviewing results, and using data to inform treatment discussions helps MBC become a natural part of care.
Panelists highlighted three core strategies:
- Embed MBC into regular clinical routines and meetings
Zócalo Health reviews their MBC dashboards in a weekly treatment planning meeting, highlighting clients with deteriorating or stagnant trends who may need adjustments to their treatment plan or earlier follow-ups, and clients who are improving, as a way to recognize clinicians’ impact and provide positive reinforcement.Regularly seeing and discussing the data makes MBC feel like a core part of delivering care, not an add‑on. - Use data to highlight clinical wins and early risk identification
Emily emphasized that when clinicians at TLC see how measures help them identify risk earlier and break through repetitive sessions by bringing clarity to what a client is actually experiencing, it becomes easier to keep clinicians engaged because they can connect the data to visible impact. - Normalize MBC in supervision and peer learning
Discussing measures and trends in supervision and encouraging clinician champions to share success stories with peers can empower clinicians to continue using MBC and achieve better outcomes.
At The Lincoln Center, how has the clinical teams perspective shifted, if at all, on their excitement surrounding MBC since launch?
Before implementing MBC, many clinicians at The Lincoln Center were concerned that it would add to their administrative workload and potentially interfere with therapeutic rapport.
Once TLC began using Greenspace, the organization made intentional choices to position MBC as a clinical support tool rather than a performance metric. Baseline measures are collected through the EMR and then entered into Greenspace, allowing clinicians to access richer dashboards and longitudinal trend lines without introducing additional complexity. Wherever possible, workflows are automated, and the use of data is intentionally embedded into weekly supervision, clinical formulation, and collaborative treatment planning.
Over time, Emily has observed a clear shift from initial skepticism to a more curious and positive mindset among clinicians. MBC is now viewed as a way to strengthen clinical judgment, bring greater clarity to complex cases, and support more informed conversations with clients, schools, and community partners. With ongoing training and peer support, clinical staff are able to address remaining concerns together and continue learning as part of their day-to-day practice.
What clinical settings seem to have the greatest client engagement, and which settings have the least?
The strongest client engagement is typically seen in settings where MBC is clearly embedded throughout the care journey and framed as a collaborative process with the client, rather than something done to them. Programs and clinicians who review results in nearly every session, using them to set agendas, revisit goals, and guide conversations, tend to see higher engagement and greater client reflection on their scores. Offering flexible completion options, such as SMS, email, or in-clinic kiosks, also supports engagement by allowing clients to complete measures in a way that fits their preferences and schedules.
Engagement is often lower when assessment completion is treated primarily as an administrative requirement or when results are not meaningfully discussed in sessions. In those situations, clients may struggle to see how measures benefit their care, and clinicians may be less consistent in assigning and reviewing assessments. Aligning MBC with supervision, program expectations, and a clear, shared understanding of its clinical value can help close this gap and drive stronger engagement across settings.
Leveraging MBC Data and Insights
What are the most useful and impactful ways to leverage MBC data?
Zócalo Health described three main cases of how they leverage their MBC data for the greatest impact:
1. Making High-Risk Populations Visible
- MBC reveals patients who are typically unseen by health plans due to low utilization or difficulty engaging.
- Registry flags identify deterioration or stagnation early, enabling accelerated follow-up or psychiatry review.
2. Early Identification Across All Entry Points
- Universal screening gives immediate insight into unmet mental health needs across medical, social-care, and therapy pathways.
- Case-ness scores allow same-day/next-day therapy scheduling for high-need members, reducing delays that drive dropout in Medicaid populations.
3. Operational + Payer Impact
- Real-time data improves case review, supervision, escalation decisions, and integrated care coordination.
- Standardized outcomes provide objective evidence of program effectiveness, supporting trust, contract expansion, and strategic planning.
- MBC enhances visibility into population needs in rural and semi-urban Latine communities; areas historically underserved due to geography, work schedules, and language barriers.
How can organizations measure the success of their MBC implementation?
Success can be measured by whether MBC is both meaningfully improving care and fitting naturally into day-to-day practice.
At the client level, this includes tracking changes in outcomes over time and using that data to inform timely treatment decisions. Clear visibility into trends helps care teams recognize when treatment is effective, when adjustments are needed, and when additional support may be required.
At the provider level, successful implementation is reflected in consistent, confident use of MBC across caseloads. Organizations look for evidence that clinicians are regularly reviewing data, bringing insights into sessions and supervision, and using results to guide clinical conversations. When MBC becomes an integrated part of routine care, rather than a separate task, it is a strong signal that implementation is working.
At the organizational level, leaders assess how effectively MBC data supports quality improvement, accountability, and the demonstration of impact to stakeholders and funders. This includes using aggregated insights to monitor engagement, identify gaps in care, and communicate outcomes internally and externally. Over time, successful implementation is reflected in stronger alignment across teams, clearer visibility into outcomes, and a shared understanding of how data drives better care.
Selecting and Administering Assessments
How do you decide the number of assessment tools to use?
Both panelists recommended starting with a small, core battery of assessments, then layering on additional measures where they add clear clinical value.
At Zócalo Health, every individual is universally screened at entry using the PHQ-9 (depression), GAD-7 (anxiety), and PREPARE (social determinants of health). The PHQ-9 and GAD-7 are embedded into intake and follow-up workflows and triggered automatically at defined intervals. PREPARE is administered at admission, six months, and one year—rather than at every visit—striking a balance between capturing meaningful change and minimizing respondent burden.
At TLC Wellness, all clients aged 12 and over complete the PHQ-9 and GAD-7 at baseline through the EMR. They also incorporate child and adolescent measures, such as the PSC-17 (child emotional and behavioural changes) and RCADS (child depression and anxiety), to ensure developmental relevance. Clinicians can add problem-specific tools as needed based on clinical judgment and client presentation.
Greenspace offers over 400 mental health assessments that address a wide range of conditions, symptoms, and demographic needs. We recommend starting with a small set of standardized assessments across programs to support reporting requirements and organization-wide learning. From there, giving clinicians the flexibility to add additional measures tailored to individual clients helps ensure a truly client-centered approach—one that captures each person’s unique goals, experiences, and challenges.
How often are you administering assessments?
The frequency with which assessments are administered depends on several factors, including the assessment author’s recommendations, session frequency, and the provider’s clinical judgment.
Dr. Elizabeth Connors from the Yale MBC Collective recommends incorporating routine assessment check-ins at the beginning of each session, with no more than one month between measures. This approach allows both clients and clinicians to fully integrate MBC into the care process—using assessments to surface experiences, guide session focus, and inform ongoing treatment decisions.
Is there a list of outcome measures that are available in Spanish and other languages?
Yes. Greenspace supports many translated measures across a wide range of languages, including Spanish for commonly used tools. Language availability depends in part on publisher permissions and the availability of validated translations, but our assessment library already includes many multilingual options.
As part of implementation planning, the Greenspace team can work with you to identify which translated tools best align with the populations you serve and ensure they are configured correctly. These can also be paired with a multilingual client dashboard, allowing individuals to view their results and complete assessments in the language they are most comfortable using.
How do you manage the risk related to responses on the PHQ-9 question 9 (thoughts of harming self) being sent to clients outside of a clinical encounter?
Managing risk around suicidality involves both thoughtful workflows and clear clinical protocols. For example, Greenspace’s Caseload Assistant surface’s suicidality flags and highlight clients that are at risk who may need additional or immediate attention. This ensures that individuals who exhibit signs of suicidality when completing the assessment outside of a clinical encounter will be flagged immediately for further intervention.
Organizations may choose whether or not they wish to have clients access their own results. It’s important to note that clients are submitting these responses themselves, and are thus aware of the information they are providing. By giving clients direct access to their results, they have the information they need to easily share their lived experiences, better understand and respond to their ups and downs, and better advocate for themselves and their needs throughout treatment.
For more information about administering and responding to PHQ-9 scores, please visit our PHQ-9 assessment guide.
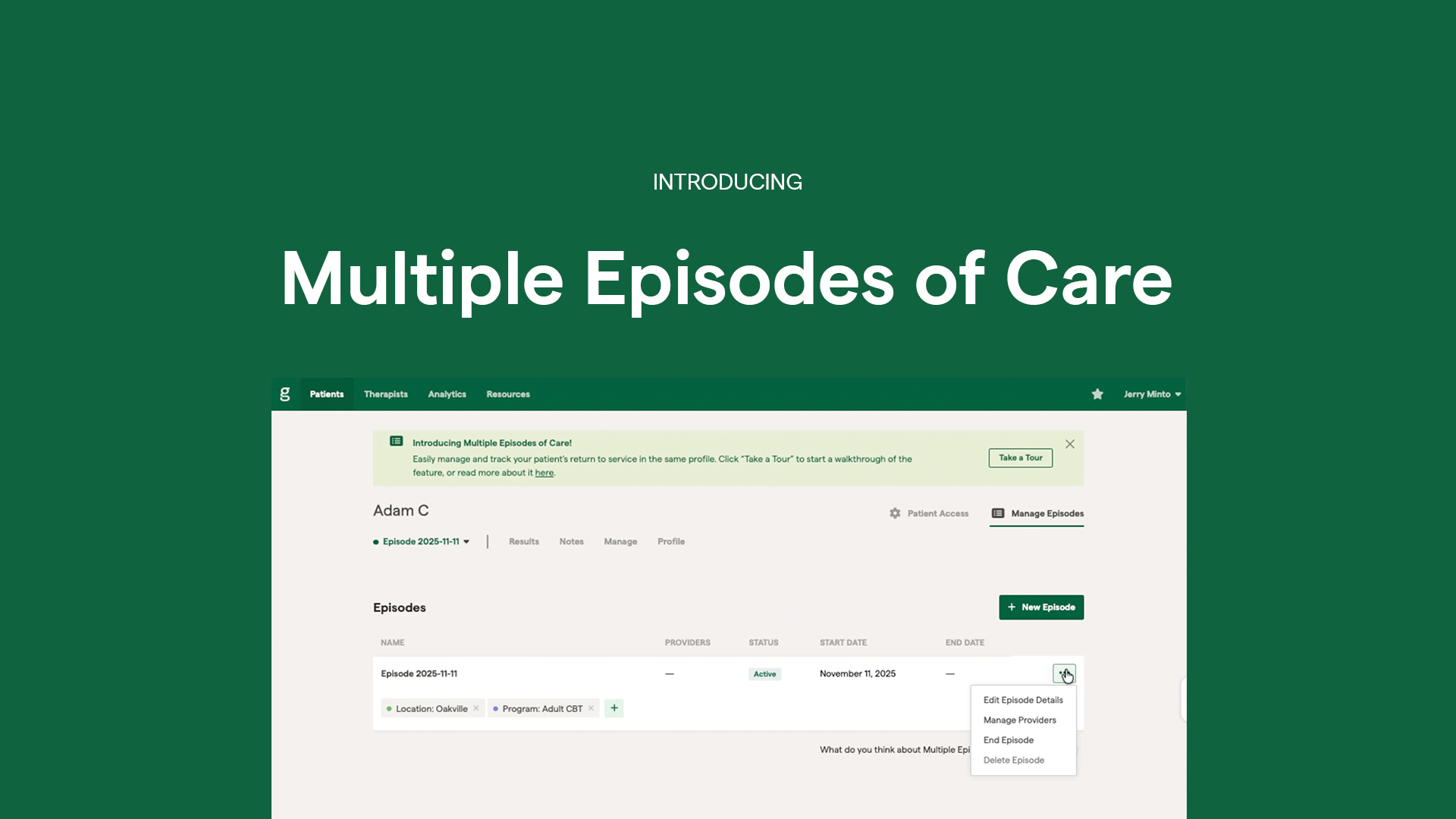
The Greenspace Platform and Implementation Support
What does the implementation support provided by Greenspace look like when starting?
As Carly outlined during the session, implementation support is designed to be structured and collaborative. It typically begins with a discovery and design phase, where we work together to understand your programs, workflows, reporting requirements, and existing technology. From there, we define a minimal core set of measures to apply across services and configure assessment schedules, high-risk protocols, client enrollment workflows, and a branded experience that reflects your organization.
Training focuses on two key areas: the practical “how” of using the platform and the clinical “why” of integrating results into sessions. Leaders and supervisors receive orientation to dashboards and KPIs so they can reinforce new workflows in day-to-day operations. For organizations that choose to integrate with an EHR or EMR, Greenspace also coordinates the planning and technical work needed to automate data exchange, with privacy and security as central priorities.
How has Greenspace integrated with your EHR?
The Greenspace platform integrates with more than 85 EHR and EMR systems and can work with nearly any clinical system. Through secure, bi-directional integrations, assessment data collected in Greenspace can flow automatically into the EHR, eliminating duplicate data entry and reducing administrative burden for clinicians and staff.
This approach allows providers to continue working within their primary system of record while benefiting from Greenspace’s purpose-built tools for outcome measurement, visualization, and clinical insight. Integrations are flexible and configurable, supporting workflows across outpatient, community-based, and integrated care settings while helping organizations maintain accurate documentation and use data more effectively to inform care.
Learn more about the benefits of integrating Greenspace with your EHR.
What exact tables or dashboards in Greenspace can be used for clinician KPIs?
Three commonly used dashboards in Greenspace include:
- Provider usage dashboards that show which clinicians have enrolled clients, how often measures are being completed, and how consistently schedules are being followed.
- Outcome dashboards that show reliable improvement, deterioration, discharge status, and therapeutic alliance trends, often filtered by program, site, or population.
- Caseload and risk views that highlight clients who may need additional attention, such as those with sustained worsening, low alliance, or recent high risk responses.
Can you look at the Greenspace assessment availability before signing up?
Yes. You can explore our Assessments Hub to view a list of over 40 of the most commonly used assessments available on Greenspace.
For access to a complete list of available measures (we offer more than 500), or to discuss more specific needs, you can connect with our team. They can confirm assessment availability, walk through any licensing considerations, and help you determine an initial set of measures that fits your clinical context.
If there are assessment tools that are not provided by Greenspace, can they be added?
Yes. Greenspace regularly adds new assessments based on partner needs and best practices. If your organization relies on a tool that is not currently in the library, our team can often configure it within your instance, subject to licensing requirements and permissions from the measure owner.
What are the fees for Greenspace?
Pricing is tailored to each organization and takes into account factors such as the number of providers, programs and levels of care, implementation scope, and whether an EHR integration is included. This flexible approach allows organizations to adopt MBC in a way that fits their size, structure, and goals.
Please Schedule a call with the Greenspace team to learn more about pricing and how we can best support your MBC implementation.
If you’re interested in learning more about implementing MBC at your organization, Schedule a call with an implementation specialist, or reach out anytime at info@greenspacehealth.com.