When it comes to mental health services, meaningful engagement from clients can make all the difference in a provider’s ability to deliver care that is responsive, effective, and personalized. For young adults, a demographic navigating critical developmental milestones alongside complex mental health needs, this engagement is particularly critical. Sustained involvement in their care can determine whether treatment feels relevant and supportive to them, or disconnected and ineffective. This means that for providers, the challenge is twofold: delivering high-quality treatment while also creating an environment where youth feel heard, empowered, and motivated to actively participate.
A recent publication in BMC Health Services Research, “Personalized and collaborative use of digital measurement-based care tools enhances engagement among young adults: a mixed-methods study,” takes a closer look at approaches to practicing MBC with young adults. The study aimed to understand effective strategies for leveraging MBC with this population, where the challenges remain, and how it can be used to transform care delivery for young people and their families.
Let’s dive into the key findings of this study and what it means for mental healthcare services catered towards young adults.
Key Findings
1. The majority of young adults see clear benefits in the use of MBC in mental health services.
83% of participants saw the value of MBC and perceived that digital tools, like an MBC platform, could help with the process of routine symptom monitoring. They described it as a tool that improved self-awareness, helped them monitor their progress, and supported communication with their providers.
Participants emphasized the value of being informed about the purpose of MBC and the role it plays as a motivator to be an active participant in their mental health journey. One participant stated that they found this information valuable: “Just an understanding of the benefits of doing measurement-based care, understanding what’s going on. Knowing the value of doing a survey and what it’s going to achieve? I’m going to therapy voluntarily, and I want to get better. That’s going to motivate me towards doing it.”
2. Collaborative review of data is a strong motivator.
The most impactful tactic for keeping youth engaged was reviewing MBC data collaboratively in session. All participants wanted to review the data during sessions and throughout treatment, and wanted to be actively involved in clinical decision-making. This collaborative process gave young adults a sense of being heard and validated, and turned raw numbers into meaningful conversations about their care.
Most participants were hesitant to initiate discussions, but when outcome data could be reviewed together, clinicians are empowered with a base knowledge of the presenting symptoms and issues. This additional knowledge can help them start a conversation that provides deeper insight into the client’s experiences and insights.
This collaborative process shifts the dynamic from provider-driven to a collaborative partnership, where young adults are not just recipients of care but active contributors to decision-making. When youth see that measures reflect their own goals, and that their responses directly shape the care they receive, they are far more likely to stay engaged and feel empowered in their treatment. Dr. Amber Childs from the Yale Measurement-Based Care Collaborative (YMBCC) uses MBC in her practice to empower her young clients. She shares that the assessments and results give youth ownership over their care process and ensures that their voices are central to treatment planning.
3. Personalization is key to sustained engagement.
Young adult clients reported disengagement when the measures felt irrelevant or too generic. If clinicians relied too heavily on the data, or the data interpretations didn’t align with their personal goals or lived experiences, they were less likely to continue participating. The study emphasizes the importance of selecting measures that feel meaningful for each individual, and using the data collected to inform discussions during sessions to get a deeper understanding of the client’s symptoms and experiences, rather than relying on outcome data alone.
Dr. Amber Childs shares guidance for clinicians curious about choosing the right measures for each client. By assigning measures that are relevant and meet the age, needs, and goals of each client, providers can help youth stay engaged and invested in their care journey.
4. Consistency and transparency of data collection and usage increases engagement.
Engagement was highest when participants understood how their data was being used. When clinicians explained what their scores meant and how they would inform decisions, young people felt more motivated to consistently complete assessments and more confident in their ability to influence their own care. Having full visibility to their own outcome data empowers clients to better understand their symptoms and communicate their needs effectively.
5. Digital design features make a difference.
Participants highlighted how digital platforms could enhance accessibility and engagement, including:
- Customizable dashboards to help them track the outcomes that mattered most;
- Visual data displays that made trends easy to understand and highlight progress;
- Reminders and notifications to support consistency and positive reinforcement;
- Interpretation and visualization support to help them connect scores with real-world meaning.
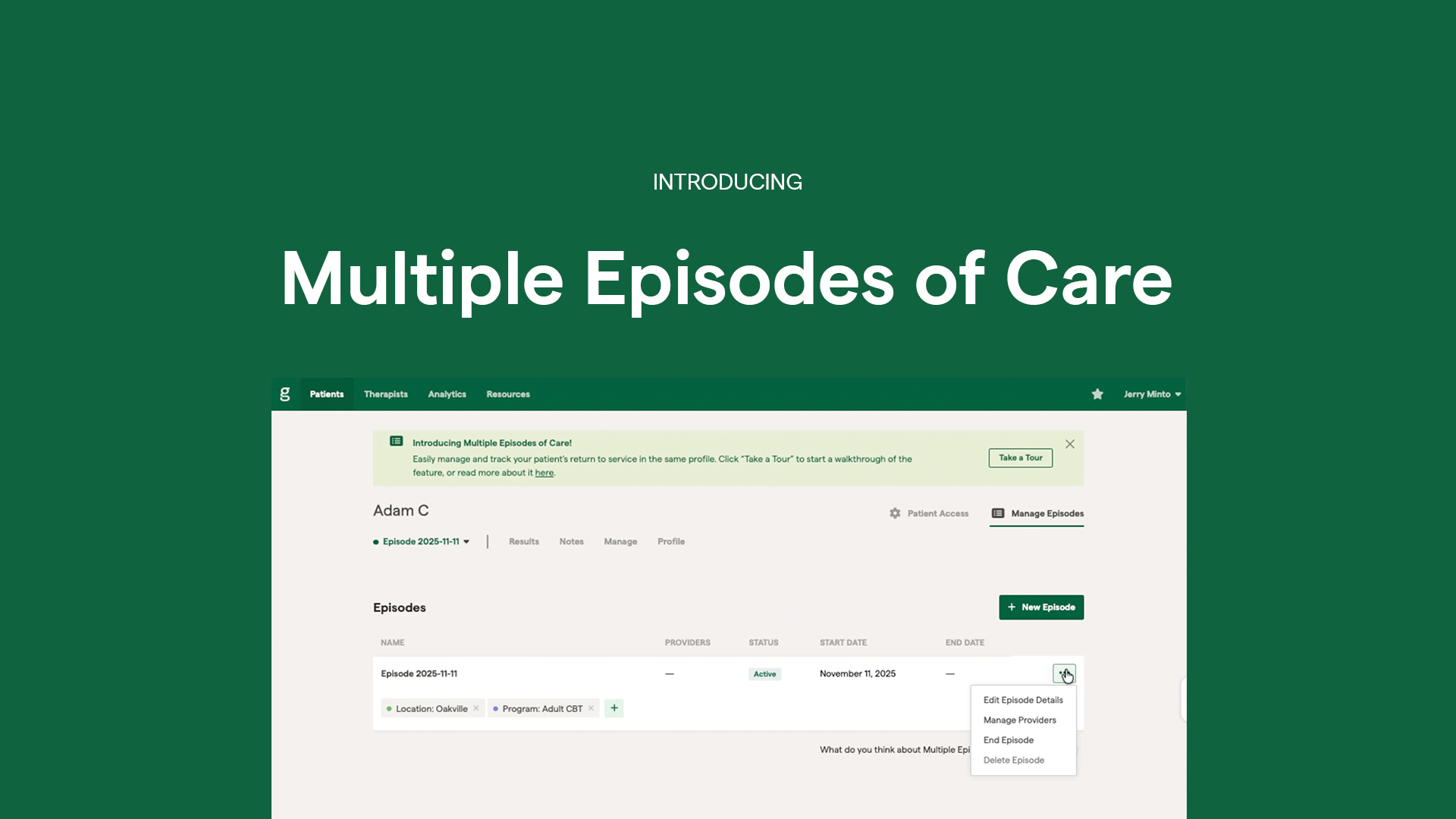
These features not only improved usability but also reinforced a sense of control and ownership over their mental health journey. The Greenspace platform is designed to deliver on these needs by providing an intuitive, client-friendly experience that makes outcome tracking engaging and meaningful. With visual reports that bring data to life, built-in reminders to encourage consistency, and flexible assessment delivery via email or SMS, our MBC solution makes it easy for clients to complete assessments, review their results, and engage with their personalized treatment pathway.
Wrapping Up
This study highlights a simple but powerful truth: MBC is not only about collecting data, it’s about meaningfully using the data to inform clinical discussions, personalize treatment, and collaboratively guide their care process.
As young people navigate complex developmental, social, and emotional challenges, engagement is everything. Across all age groups and populations, when MBC is implemented in ways that feel personal, collaborative, and transparent, it strengthens therapeutic alliance, empowers clients to take an active role in their care, and ultimately improves outcomes.
Interested in learning more about how MBC can enhance mental healthcare services for your population? Schedule a call with one of our implementation experts or reach out to us anytime at info@greenspacehealth.com.
References
Chong, M.K., Hickie, I.B., Ekambareshwar, M. et al. Personalized and collaborative use of digital measurement-based care tools enhances engagement among young adults: a mixed-methods study. BMC Health Serv Res 25, 752 (2025). https://doi.org/10.1186/s12913-025-12889-1