Measurement-Based Care (MBC) is widely recognized as a key component of delivering high quality mental and behavioral health care. In fact, tracking progress throughout care is one of the most influential predictors of positive treatment outcomes. It’s been shown to support clinical decision making, enhance client engagement, and improve therapeutic alliance.
One of the most significant factors that contribute to the success of MBC is using patient-reported outcome measures (PROMs) in collaboration with the client. This involves routine assessment completion, discussing scores with clients in session and getting curious about symptom changes that stand out by asking clients open-ended questions to help develop a deeper understanding of their challenges, their experience in care and their personal treatment goals. This process allows clients to better understand their mental health, uncover symptom change patterns, and empowers them to further engage as partners in their care process.
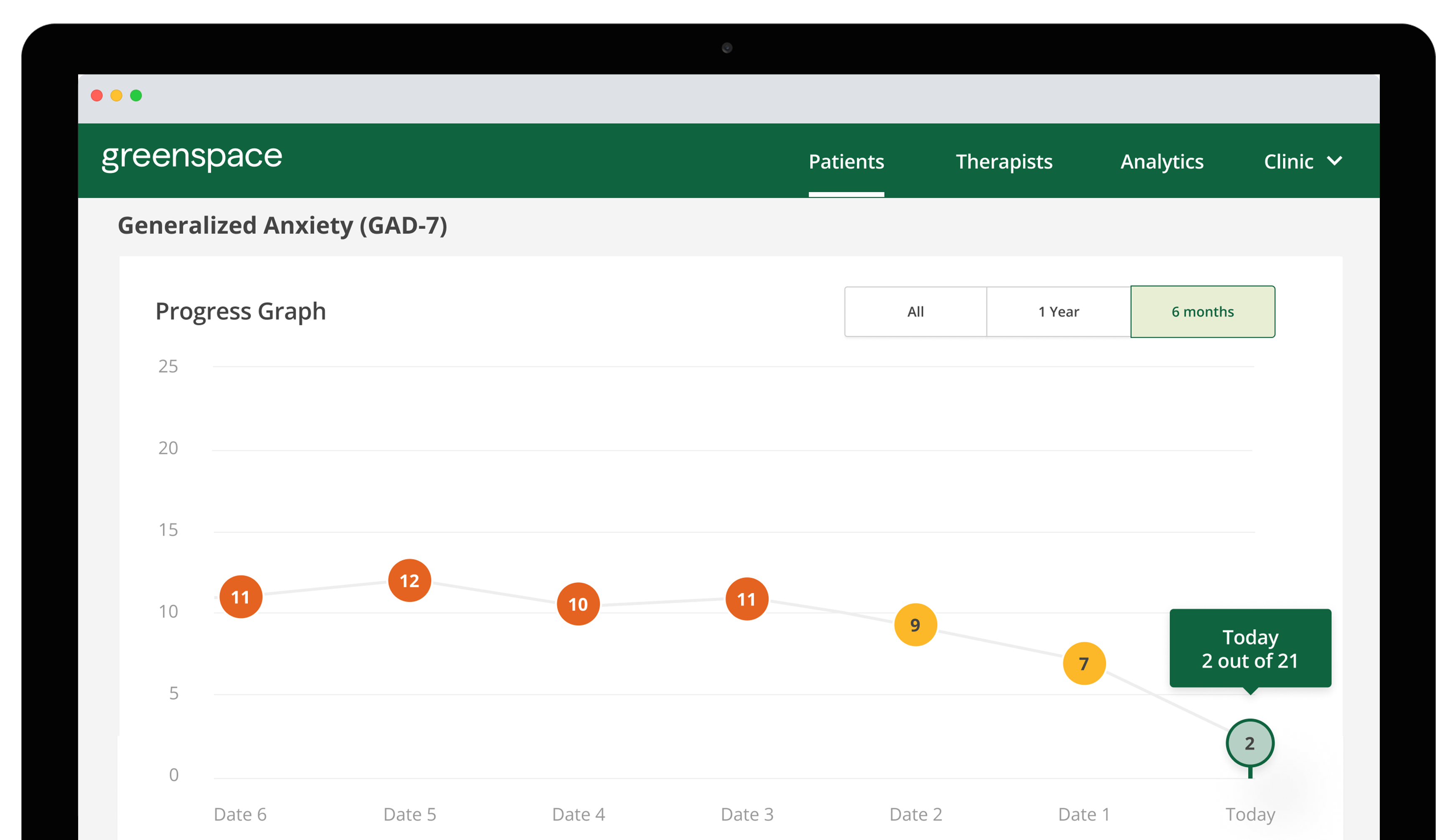
The positive impact of MBC on clients is further elevated when they’re given full visibility into their results. As an example, people in care with a clinician that is using Greenspace are able to log in and view their own results dashboard, where past and current assessment scores are linearly displayed using intuitive visuals and graphs. We have witnessed firsthand the positive effects that providing clients access to their own results can have on their overall experience and outcomes (Naomi Richter’s story for example), and there is a wealth of evidence supporting the clinical utility of direct client feedback. With access to their own data, clients can track their ups and downs, identify areas for improvement, and reflect on the progress they’ve made (especially important to help provide hope during more difficult days).

After introducing Greenspace to our clients, we found that they were empowered by the ability to track their own progress, instead of just being told if they were progressing or not. I’ve learned that encouraging clients to participate in their own tracking provides additional self-awareness, which is key in the recovery process.
Transparency and direct client feedback are two of the most important elements of Measurement-Based Care that impact quality of care and outcomes. To ensure your MBC process addresses both, there are a few important elements to remember when implementing and leveraging MBC in practice:
1.MBC creates an opportunity for clients and clinicians to collaboratively re-evaluate the treatment plan. MBC is a clinical tool and process that can be used to share progress towards clinical goals with clients and collaboratively re-evaluate treatment plans or approach whenever needed. There’s shown to be a distinct difference in outcomes when only the clinician is given access to results versus both the clinician and client, where the client+clinician group saw the highest percentage of clients experiencing reliable or clinically significant change (64% vs 57%) in their symptoms (Hawkins et al., 2004). More interestingly, when looking at clients considered not-on-track, the client-clinician feedback group saw 2x more clinically significant change (23% vs. 10%) than the clinician-only feedback group (Hawkins et al., 2004). Collecting data on patient outcomes is great, but there’s evidence of the meaningful additional value that is created by providing clients with direct access to results and discussing and exploring their meaning together.
2. MBC empowers the client to effectively understand and communicate about their own symptoms and experiences to inform their treatment goals and decisions. Providing clients with a concrete way to visualize their own symptoms empowers them to become a driver of their care, engage in the care process and better understand their mental health journey. By providing clients visibility into their results, they’re given additional tools to learn about their own well being. They can see the areas they’ve made progress, and identify what factors impact their symptoms positively or negatively which can help them see better results throughout care and build resilience outside of the care setting. This stronger sense of self-awareness enhances a client’s ability to engage in conversations with their clinician, allowing them to become more knowledgeable about their own mental health, their progress, and the impact treatment is having on them.
3. MBC enhances the client’s ability to self-identify when they are off-track. It’s easy for clients to recognize when they are off-track when given insight into their treatment progress. It’s one thing to ‘feel off’ and try to communicate that to a clinician but, when clients can easily identify changes in their own data throughout therapy, it strengthens their ability to self-monitor while in treatment, and provides a shared language to easily communicate their experience in session. Research shows that progress presented in written and graphic form can increase the impact of the clinician feedback on clients, whereas verbal feedback alone has less of an impact (Harman et al., 2005). By giving clients direct access to their results, they have the information they need to easily share their lived experiences, better understand and respond to their ups and downs, and better advocate for themselves and their needs throughout treatment.
4. MBC fosters equitable care delivery. A person’s Background, education, comfort, and familiarity with mental health treatment can play a major role in a clients ability to express themselves in the therapy room. MBC is designed to prioritize the clients voice, so they can feel comfortable communicating their needs and experiences, advocating for themselves, and ultimately benefit from their treatment. Empowering clients with the knowledge and tools to communicate with their provider is fundamental to delivering equitable and culturally sensitive services.
Final Thoughts
Visibility into Measurement-Based Care assessment results allows treatment to go beyond verbal communication and solely qualitative communication of experiences. It empowers clients in treatment, improves their engagement in the care process, and contributes to a higher therapeutic alliance— as clinicians can ensure they’re addressing the evolving needs and goals of their clients.
To learn more about the benefits of client visibility or to see our client dashboard in action, visit greenspacehealth.com to book a call with one of our MBC implementation experts or email us anytime at info@greenspacehealth.com.
References
Harmon, C., Hawkins, E. J., Lambert, M. J., Slade, K., & Whipple, J. L. (2005). Improving outcomes for poorly responding clients: The use of clinical support tools and feedback to clients. JCLP/In Session, 61(2), 175-185. 10.1002/jclp.20109
Hawkins, E. J., Michael, L., & Vermeersch, D., & Slade, K. L., & Tuttle, K. C. (2004). The effects of providing patient progress information to therapists and patients. Psychotherapy Research, 14(3), 308-327. 10.1093/ptr/kph027
Further learning:
D’Costa, S.N., Kuhn, I.L. & Fritz, Z. (2020). A systematic review of patient access to medical records in the acute setting: Practicalities, perspectives and ethical consequences. BMC Med Ethics, 21(18). https://doi.org/10.1186/s12910-020-0459-6
Krägeloh, C., Czuba, K., Billington, R., Kersten, P., & Siegert, R. J. (2014). Using feedback from patient-reported outcome measures in mental health services: A scoping study and typology. Psychiatric Services, 66(3), 224-241. 10.1176/appi.ps.201400141.
Greenspace Health. (2022, February 15). Talking to Clients About Measurement-Based Care. https://greenspacehealth.com/talking-to-clients-about-measurement-based-care/.
Related Resources