Our Population Health Hubs are setting a new standard for mental health support across any large population. The Hubs provide all people in need of support with a one-stop-shop digital front door to easily navigate and access all available wellness resources.
Inspired by the evidence surrounding transformational impact of Measurement-Based Care in a clinical setting, we built our Population Health hubs to empower users with personalized self-guided mental health tracking to help them get curious about their ups and downs and better understand their overall mental health. This feature empowers people to take a more active role in their mental healthcare and increases engagement with preventative resources and retention within services, while also driving significant symptom improvement. As a direct result of users completing bi-weekly patient reported outcome measures (PROM’s), organizations (health systems, insurers, payors, unions, businesses, campuses, etc.) are equipped with the usage and outcome data needed to better understand their population’s needs, reduce their overall costs of care, and drastically improve the quality of their mental health supports and wellness strategies.
Let’s breakdown how our Population Health Hubs work to set a new standard of care for the population that your organization or system supports:
1. The Pop Health Hub improves navigation to care that is most relevant to each individual.
When supporting the mental health of large groups of people— whether that is constituents within a health system, students on a campus, or employees within a business — it’s very difficult for people seeking care to be aware of all resources available to them. Beyond knowing what’s available, it’s difficult for people to identify which resource(s) may be most appropriate for their needs and how to access them within large and complex systems.
As a result of difficult navigation, many people traditionally access 1:1 in-person care first, despite it often not being the most appropriate option for their needs, or their first interaction with the mental health system ends up being a visit to the emergency room while in crisis. Not only does this create longer wait times for services and drastically increase costs of care, it prevents people from accessing upstream services (e.g., Self-Guided iCBT, Group Therapy, Mindfulness Apps etc.) that can help people with mild or moderate mental health challenges proactively maintain or improve their mental health to prevent future challenges. Without the opportunity for early intervention, we increase the likelihood of more acute mental health struggles down the line, which are associated with higher-cost behavioral and physical health services. Evidence shows that those suffering from mental health challenges see a 60% increase in costs for physical health services compared to those with the same physical condition who are not accessing high-quality services to address their mental health challenges (Clark & Layard, 2014). Additionally, about 40% of people with anxiety and depression are also facing a long-term physical health problem, and the cost of managing their physical health is about 50% higher compared to those with the same physical conditions who are not experiencing mental health challenges.
After over 250,000 users have accessed services through one of our Population Health Hubs, the results are promising. Our hubs show that when alternative self-guided resources are available, 70% of individuals choose to access lower-cost, self-guided resources first instead of 1:1 counselling services.
This has significant implications on both clinical outcomes and wait times, as individuals can access the resources they need while also ensuring that 1:1 care is available to those who need it most, right when they need it.
2. Account creation and self-assessments drive long-lasting engagement and drastically increase retention.
While there is an abundance of mental health apps and online services available today, they often struggle to maintain user engagement over time. In 2019, a systematic review was conducted on 93 mental health apps and found a median 15-day retention rate of approximately 4% of total users and a 30-day median retention rate of 3% of total users. If you compare that to the retention rates across our Population Health Hubs, there’s a significant difference; our 15-day and 30-day retention rates are 46% and 43%, respectively. So what is it that keeps users so engaged?
Two main areas contribute to high engagement across our Population Health Hubs:
- Sign-up Conversion – While users are not required to sign up to access resources, in order to complete regular self-assessments and monitor their mental health progress, users are prompted to create an account. For all users landing on the Hubs main page, the sign-up conversion rate is 17%, which is well above the industry standard of approximately 3-6%. This tells us that users value what the hub offers, specifically personalized insights drawn from their bi-weekly assessment results.
- Self-assessments – If we break down our 30-day retention rate of 43% a bit further by removing users who do not complete a self-assessment, we’re still left with a 39% retention rate. This means 93% of our users who return to the platform come back to complete their self-assessment and access their visual results and insights.
High engagement and retention increases the use of proactive and self-guided resources and helps to reduce wait times for 1:1 care— ultimately improving the mental health of the population being served and reducing their overall costs of care. We know from the evidence behind Measurement-Based Care that consistent and frequent assessment, alongside visibility into results, contributes to higher engagement in care and higher symptom improvement in clinical settings, so what happens when we empower populations with the same opportunity in a self-guided setting?
3. Bi-weekly assessments empower individuals to track their symptom changes, enhancing their personal understanding of their mental health and improving outcomes.
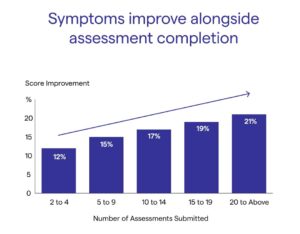
Similar to results seen in clinical applications of Measurement-Based Care, when we allow individuals to track their mental health symptoms, we empower them to reflect on positive and negative contributors to their well-being. This process helps them better understand their mental health and what impacts it, as well as identify when they may need further support. Our Population Health Hub outcome data shows that, regardless of the resource users access, the more assessments an individual completes, the more their symptoms improve.
Akin to the impact of Measurement-Based Care in a clinical setting, it’s clear from both qualitative user feedback and quantitative outcome data that providing self-guided users the ability to track and understand their mental health outcomes drastically improves engagement and helps to significantly reduce mental health symptoms.
4. Care Management and high-risk flags encourage participation in upstream resources to ensure all people have access to the support they need.
Our Population Health Hub ensures health systems and organizations are equipped to reduce critical mental health crises across the population by proactively supporting at-risk users across their care ecosystem. Regular assessments help ensure individuals are prompted to engage with the most appropriate resources or services early on to avoid deterioration and decrease the need for higher levels of care. If an individual’s symptoms start to deteriorate, become severe, or they indicate signs of suicidal ideation, automatic high-risk flags are made available to Case Managers, who can proactively reach out and guide them to the resources or services that are most appropriate to address their immediate needs.
5. Health Systems and organizations can leverage outcome data to empower evidence-informed learning, and improve resourcing and strategic decision-making.
Empowering your population with mental health outcome tracking (Patient Reported Outcome Measures or PROMs) generates a powerful and objective data set for the supporting health system or organization. With the ability to filter data by any subset— including age, demographic, ethnicity, gender, sexual orientation, and more—systems and organizations can now easily leverage evidence-based insights and service gaps to inform and improve their support services and mental health strategy.
Which resources is your population choosing to access? What is the effectiveness of each resource? Where might there be service/resource gaps across your population or within subsets of the population you support? All of this information is now available to inform resource improvements, mental health support strategy iteration, and program innovation to better support population-level mental health and reduce the overall cost of behavioral and physical healthcare.
Final Thoughts
As we continue to respond to a rapid and consistent increase in demand for mental health services, alongside a shortage of mental health professionals, it’s clear that we need to innovate our strategy to how people access services across large populations. This approach should make navigating and accessing services easier than ever before, while empowering people to better understand their mental health and take more agency throughout their care journey.
When we leverage the benefits of Measurement-Based Care across health systems, we help individuals thrive and ensure that health systems and large organizations have the data necessary to inform innovation to drastically improve the quality and impact of available supports and resources. Empower your community with a digital front door through our Population Health Hubs, setting a new standard for population-level mental health support.
To learn more about our Population Health Hubs, or to dive deeper into the impact they’re having across North America, book a call with one of our implementation experts or reach out anytime at info@greenspacehealth.com.
Related Resources