Mastering CMS Medicare Star Ratings: A Strategic Guide for Medicare Advantage Leaders
- What are Medicare Star Ratings?
- The Financial Impact of Star Ratings
- The Mechanics: How CMS Star Ratings Work
- Key Measurement Tools in the Star Ratings System
- The Role of HEDIS, CAHPS, and HOS in Medicare Star Ratings
- Strategies to Address High-Impact CMS Star Measures
- How to Improve HEI, CAHPS, HEDIS, HOS, and Star Rating
- Leveraging Population Health Platforms to Improve Star Ratings
- Boost Your Star Rating with Population Health
In today’s competitive landscape, Centers for Medicare & Medicaid Services (CMS) Star Ratings are more than a measure of quality for Medicare Advantage Organizations (MAOs), they’re a critical driver of growth, revenue, and long-term sustainability. Each year, the CMS releases updated Star Ratings for Medicare Advantage (Part C) and Medicare Prescription Drug (Part D) plans, based on performance data from two years prior. Designed to help Medicare beneficiaries compare the quality and performance of plans, these ratings ultimately influence plan enrollment, Quality Bonus Payments (QBPs), and long-term financial sustainability.
This comprehensive guide covers the core components of the CMS Star Ratings system, the impact of member experience, the financial implications tied to performance, and practical, data-driven strategies for improving scores through a holistic population health solution.
What are Medicare Star Ratings?
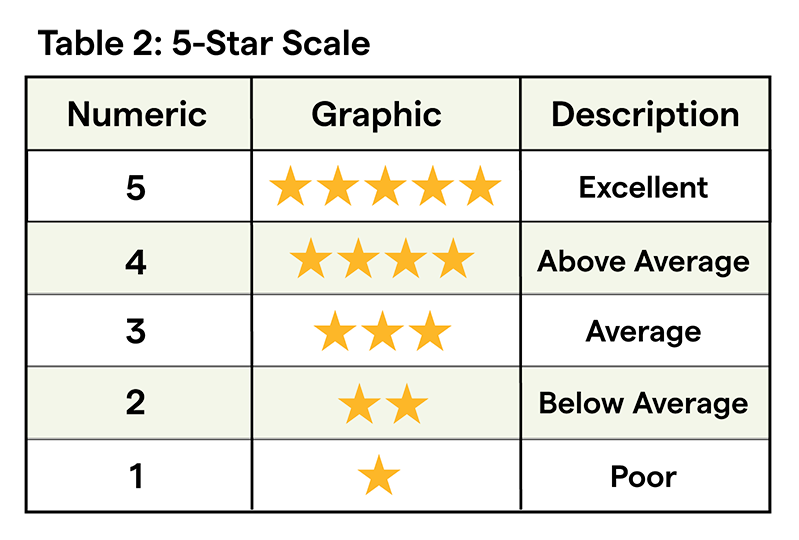
Star Ratings help Medicare beneficiaries compare the quality and performance of health plans during open enrollment. Ratings are published annually on Medicare.gov and range from 1 to 5 star, with half-star increments used for added precision.
Plans are evaluated across four rating levels:
- Individual Measures: These are the building blocks of the Star Rating system. Each measure evaluates a specific component of quality, performance, or member satisfaction. Examples include customer service responsiveness, clinical outcomes (e.g., controlling blood pressure, diabetes management), preventive services (e.g., cancer screenings, immunizations), medication adherence, member complaints, and disenrollment rates.
- Domains: Domains group individual measures into thematic categories that reflect broader areas of plan performance. They provide a more organized look at how plans perform across specific functions. Examples include Member Experience with Health Plan (CAHPS-based), Member Complaints & Changes in Plan Performance, Health Plan Customer Service, Staying Healthy (screenings, vaccines, preventive care), and Managing Chronic Conditions (more details on these later).
- Summary Ratings for Part C and Part D separately: These summary scores help consumers evaluate health and drug coverage separately, which is useful for those enrolled in standalone drug plans or MA-only plans. They include composite scores that roll up all applicable domains into two separate ratings:
- Part C (Medicare Advantage): Reflects medical care quality and plan operations.
- Part D (Prescription Drug Plan): Reflects drug plan services and medication-related measures (e.g., adherence, customer service, drug pricing accuracy).
- Overall Star Rating: For plans that offer both medical and drug coverage (Medicare Advantage Prescription Drug Plans or MAPDs), CMS publishes a combined Overall Rating that reflects total performance across Part C and Part D measures. The Overall Rating is often the headline score that beneficiaries see first and is used by CMS to determine bonus payments. Plans with a 4-star rating or higher are eligible for quality bonus payments and gain preferential placement on Medicare Plan Finder.
The Financial Impact of Star Ratings
MAO’s who want to thrive in the evolving healthcare landscape must ensure that members are accessing timely, high-quality services that meaningfully improve their well being and satisfaction level with the resources and care provided to them. CMS Star Ratings have a direct influence on several priority areas:
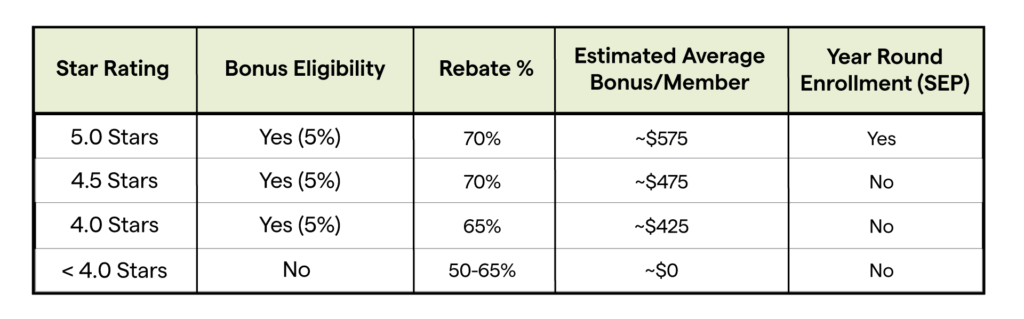
- Bonus payments: Quality Bonus Payments (QBPs) are only available to plans rated 4.0 stars and above.
- Rebate percentages: When Medicare Advantage plans submit their annual bids to CMS, they estimate the cost of providing care to their members. CMS then compares this figure to a predefined regional benchmark. If the plan’s bid comes in below the benchmark, the difference (known as the “savings”) is partially returned to the plan in the form of a rebate. The size of that rebate is directly tied to the plan’s Star Rating.
A quick example: Take a benchmark of $1,000, a plan bid of $900, and savings of $100.
A 3-star plan would receive $50 of that savings per member (50% rebate), while a 5-star plan would receive $70 (70% rebate), a $20 difference per enrollee. For a plan serving 20,000 members, that quality improvement could translate to an additional $400,000 in annual revenue, solely from rebate uplift.
These rebate dollars are critical. Plans can use them to fund supplemental benefits, reduce premiums, and invest in services that drive member engagement and satisfaction, all of which, in turn, influence future Star Ratings. It’s a reinforcing cycle: better quality drives higher rebates, which fuel better offerings and outcomes.
- Member enrollment: Plans with higher ratings see significantly higher enrollment growth, in part because Medicare offers a Special Enrollment Period (SEP) that allows beneficiaries to switch into a 5-star rated plan once per year, outside the standard enrollment windows. This SEP is available from December 8 through November 30 of the following plan year. This gives 5-star plans a competitive edge by enabling year-round member acquisition opportunities.
- Competitive edge: With an estimated $11.8 billion in bonuses distributed in 2024 alone, Star Ratings can define market leaders.
Note: About 40% of 2025 MA plans achieved ≥4 stars; 62% of enrollees are in 4+‑star plans.
The Mechanics: How CMS Star Ratings Work
To effectively maximize success and boost Star Ratings, it’s important to understand how CMS gathers, scores, and weighs Star Ratings in order to determine where efforts should be made for the greatest organizational impact.
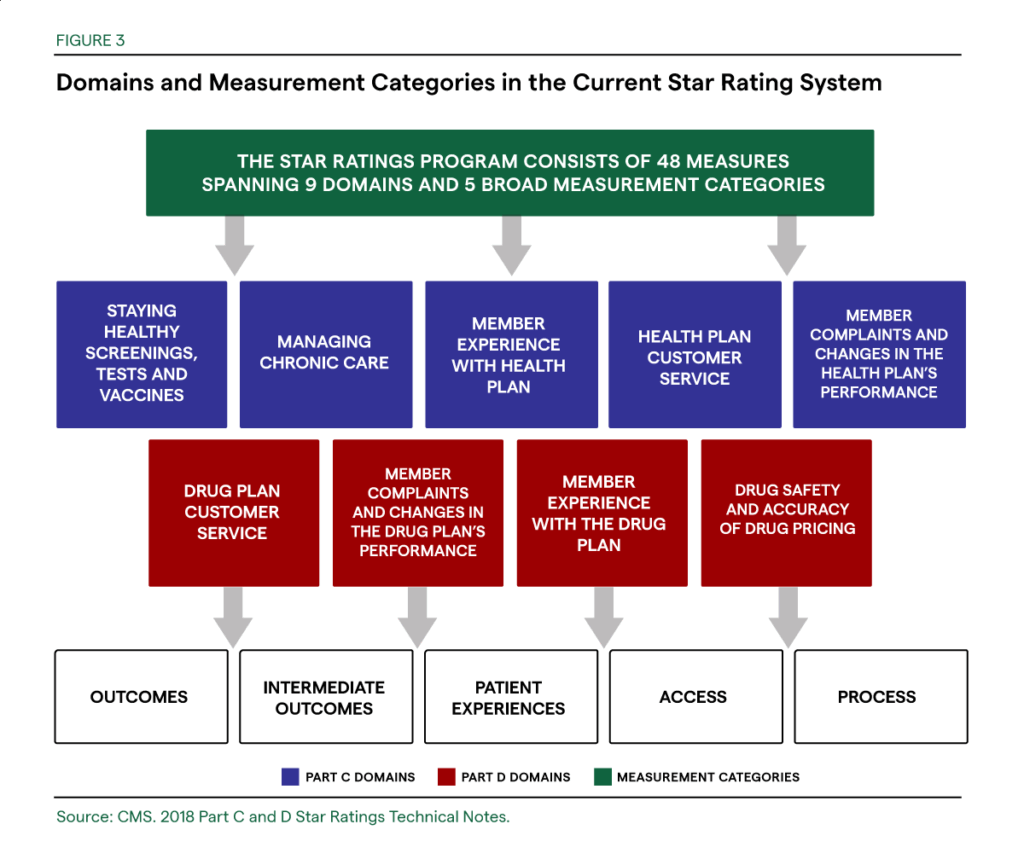
As mentioned above, Medicare Advantage (Part C) and Medicare Prescription Drug (Part D) plans are given an overall star rating, summary ratings, as well as rated based on individual measures and based on performance across five main subcategories (also referred to as Domains). The domains include:
- Member Experience: Access, communication, satisfaction.
- Customer Service: Plan responsiveness, appeals process.
- Member Complaints and Performance: Performance improvement YoY, frequency of complaints.
- Staying Healthy: Preventive care, screenings, vaccinations.
- Managing Chronic Conditions: Treatment adherence, monitoring.
Notably, Prescription (Part D) and Medicare Advantage (Part C) plans that include drug coverage are not rated on the management of chronic conditions and health maintenance, but have the addition of Drug Safety and Accuracy of Drug Pricing (i.e. How often members are prescribed medicine in a way that’s safe and recommended for their condition, and how accurate the plan’s pricing information is).
Overall, these subcategories offer more specific guidance for those looking for a new Medicare plan, where they can form a decision based on whether or not the plan excels at delivering the type of service they need. The categories offer insurance plans more insight into which areas of investment are needed in order to improve the care they have available to members and ultimately increase their overall Star Rating.
Key Measurement Tools in the Star Ratings System
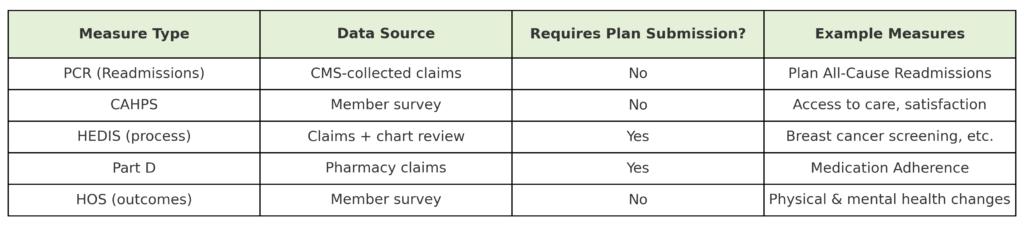
To evaluate the quality of MA plans by domain, CMS relies on a combination of survey instruments and performance metrics that assess both patient experience and quality of care.
The rating system uses more than 40 different quality measures across the categories listed above, but the most influential measures include the PCR (Readmission), CAHPS (Consumer Assessment of Healthcare Providers and Systems), the HOS (Health Outcomes Survey), and the HEDIS (Healthcare Effectiveness Data and Information Set).
By understanding what these tools are measuring and what elements are easily within an insurance company’s control, organizational leaders can tailor their offerings to ensure they’re meeting the needs of their members and providing seamless access to high-quality services and care, which are key drivers of star ratings.
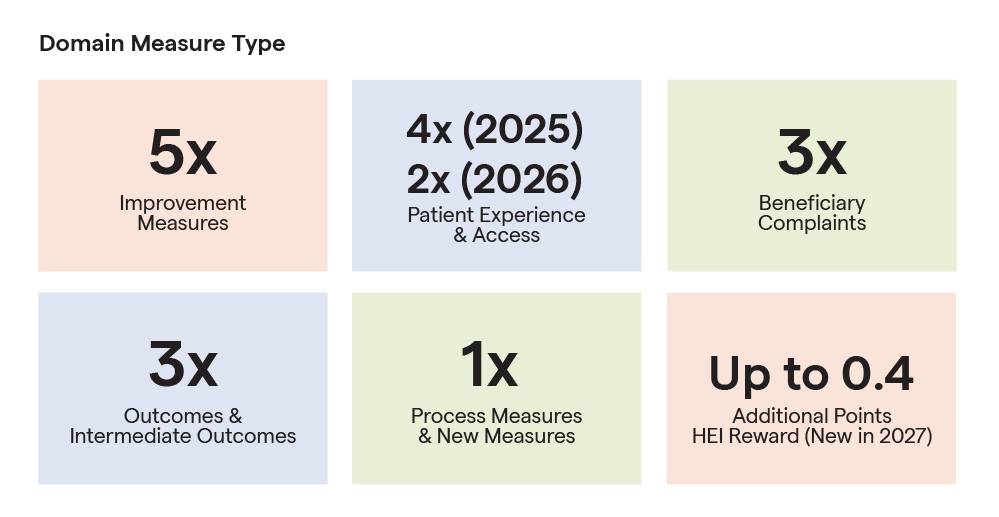
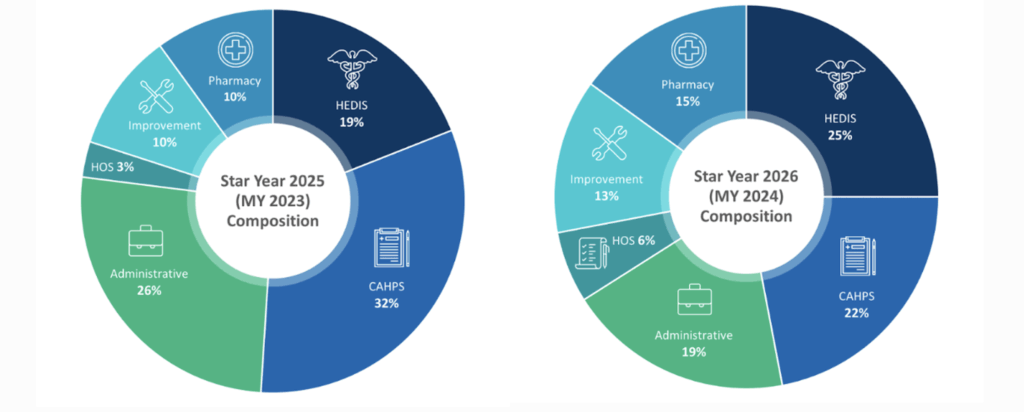
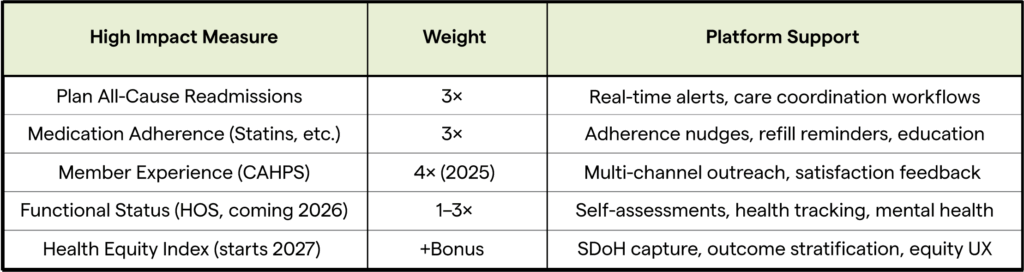
For several years, CMS heavily emphasized the importance of member perception, experience, and satisfaction in Star Ratings and bonus reimbursements. While member experience remains a key driver of star ratings, CMS reduced the weight of member experience, access, and complaints measures from 4x to 2x for the 2026 Star Ratings (based on Measurement Year 2024). This reflects CMS’s broader push to balance performance across clinical and operational measures. Importantly, CAHPS scores (which reflect member experience) aren’t limited by CMS rules that cap how much a score can change from year to year, while other measures do. CMS also now removes extreme high or low scores when calculating cut points, so one unusual result doesn’t drastically impact ratings.
Additionally, the Plan All‑Cause Readmissions (PCR) measure was increased from 1x to 3x for 2025. The PCR measure evaluates the percentage of inpatient discharges for Medicare Advantage (MA) members aged 18 and older that result in an unplanned acute readmission within 30 days. It includes readmissions for any reason, making it a comprehensive indicator of care coordination, discharge planning, and follow-up effectiveness.
Star Rating Composition 2025 vs 2026
For more on upcoming changes to CMS Star Ratings in 2026, visit this resource.
Looking ahead, CMS will introduce a new Health Equity Index (HEI) reward beginning with the 2027 Star Ratings (based on Measurement Year 2024 & 2025). This reward will recognize plans that perform well for members with social risk factors, such as dual eligibility, disability, or low-income subsidy (LIS) status. Insurers with population health tools that are equipped to capture social determinants of health (SDoH), stratify outcomes by risk group, and drive targeted engagement to help maximize HEI impact will be best positioned to benefit from HEI specific bonuses.
The Role of HEDIS, CAHPS, and HOS in Medicare Star Ratings
To evaluate the quality of care provided by Medicare Advantage (MA) plans, the CMS relies on three core measurement systems: HEDIS, CAHPS, and HOS. While each system has distinct goals and methodologies, they often overlap, particularly when it comes to incorporating patient-reported outcomes into performance measures. This integration reflects the importance of both member experience and clinical effectiveness in determining care quality.
What Is HEDIS?
The Healthcare Effectiveness Data and Information Set (HEDIS) is one of the most widely used tools in managed care, developed and maintained by the National Committee for Quality Assurance (NCQA). It consists of 90+ standardized measures across six domains, including effectiveness of care, access, and utilization. HEDIS measures are primarily based on clinical data from administrative claims and electronic medical records, but several also use survey data from CAHPS and HOS.
There are two key types of HEDIS measures:
1. Claims or Clinically Reported HEDIS Measures
These assess care delivery using medical records or administrative data and include:
- Follow-up after hospitalization for mental illness
- Depression screening and follow-up
- Medication adherence (e.g., antidepressants)
- Diabetes screening in individuals with schizophrenia
- Substance use treatment engagement
- Metabolic monitoring for children on antipsychotics
2. Survey-Based HEDIS Measures (Collected via CAHPS or HOS)
These focus on patient experience and behavior, such as:
- Getting Needed Care, Care Quickly, and Care Coordination (CAHPS)
- Monitoring Physical Activity (HOS)
- Improving Bladder Control (HOS)
- Reducing Fall Risk (HOS)
Though collected through CAHPS or HOS, these measures are still categorized as HEDIS Effectiveness of Care because they assess specific interventions and their impact on health.
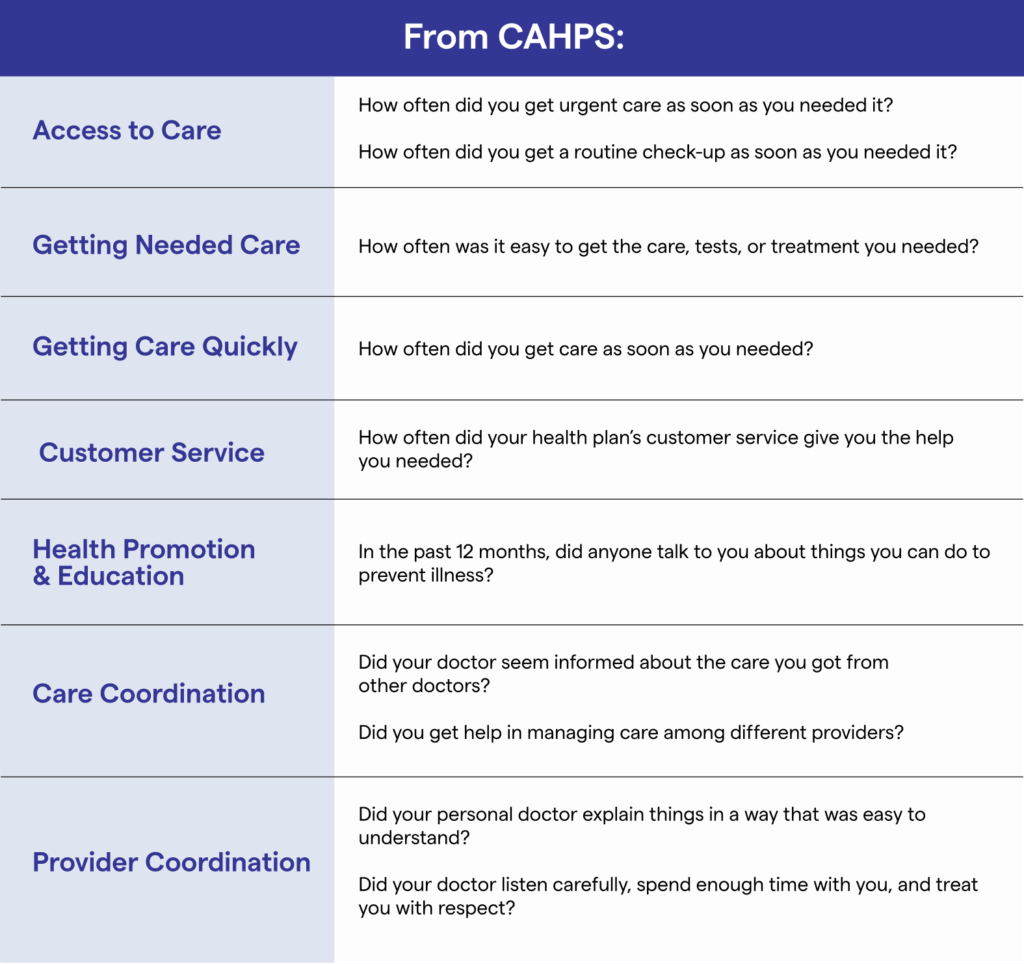
What Is CAHPS?
The Consumer Assessment of Healthcare Providers and Systems (CAHPS) is a standardized patient satisfaction survey required by CMS and NCQA. It collects feedback on the member experience with care delivery, communication, access, and coordination. CAHPS responses directly inform several HEDIS measures and also make up a distinct Star Ratings domain weighted at 2x, making it one of the most influential rating components.
Survey questions include:
- Health education and preventive guidance
- Overall satisfaction ratings (e.g., health plan, doctor, specialist, drug plan)
- Access to urgent and routine care
- Doctor communication and respect
- Helpfulness of customer service
- Care coordination across multiple providers
These insights are used to assess the quality of service from a member’s perspective, blending subjective experience with objective service outcomes.
What Is HOS?
The Health Outcomes Survey (HOS) is a longitudinal, self-reported survey required for all Medicare Advantage plans. It evaluates functional health outcomes over a two-year period by asking the same respondents to complete a baseline and follow-up survey. It is currently the only Medicare survey measuring changes in physical and mental health status over time.
HOS serves two key purposes:
1. Functional Health Measures (Regained Weight in 2025)
CMS temporarily removed the weighting of HOS functional health measures during the COVID-19 pandemic, but two of these measures: ‘Improving or Maintaining Physical Health’ and ‘Improving or Maintaining Mental Health’, regained a 1x weight in the 2025 Star Ratings. Functional Health Measures assess whether a member has improved, maintained, or declined in:
- Physical health
- Mental health
- Activities of daily living (e.g., bathing, dressing)
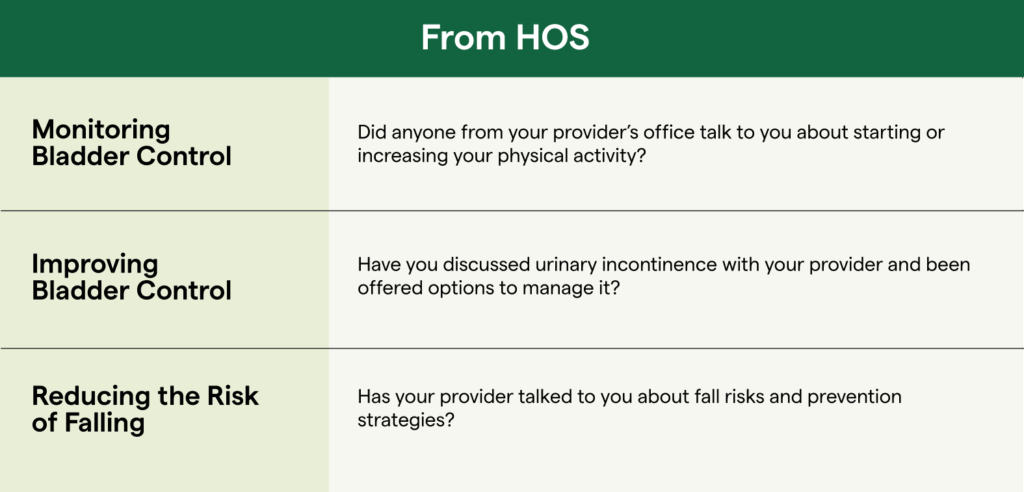
2. Survey-Based HEDIS Measures
The HOS is also used to collect data for three important HEDIS Effectiveness of Care measures:
- Monitoring Physical Activity
- Improving Bladder Control
- Reducing the Risk of Falling
These measures reflect conversations or counseling provided by clinicians, such as whether the provider discussed fall prevention or physical activity which are key quality indicators, particularly for older adults.
Population Health with Greenspace
Talk to an expert to explore how we can help boost your CMS Star Ratings.
Book a CallStrategies to Address High-Impact CMS Star Measures
To meaningfully move the needle on your Star Rating, your strategy should align with the specific questions and categories that the CMS uses to evaluate performance. Here’s a clear breakdown of the survey-based HEDIS and CAHPS questions that Medicare Advantage Organizations (MAOs) can proactively influence to improve their Star Ratings. These measures are particularly impactful because many are high-weighted (3x+) in the Star Ratings formula, meaning even small improvements can significantly affect an MA plan’s overall rating.
Survey-Based HEDIS Measures (Collected via CAHPS or HOS)
These are officially categorized under HEDIS Effectiveness of Care, but the data is collected through patient surveys (either CAHPS or HOS). MAOs should ensure care teams and member health access platforms are addressing these topics during member interactions to boost scores.
How to Improve HEI, CAHPS, HEDIS, HOS, and Star Rating
To elevate your members’ experience and outcomes, and increasing your Star Rating, here are some key strategies to that can be implemented to address the core questions and categories outlined above:
1. Enhance Access and Awareness
Tied to: Getting Needed Care, Getting Care Quickly, and HEDIS Scores
It’s imperative to make it easy for members to know what resources and services are available to them and empower them to easily navigate and access them. Offer health literacy tools, appointment and health check-in reminders, and navigation support to reduce friction. Ensure your network PCP’s and clinics understand where they can direct their patients for additional support. This helps ensure members are aware of resources and, even if they don’t access any, ensure they are more likely to report satisfaction with the services and resources their insurer offers them.
2. Deliver Responsive, Personalized Resources
Tied to: HEI, Customer Service, Health Promotion and Education, Getting Needed Care, Getting Care Quickly
Provide a resource and service navigation platform that tailors recommended content, resources and services based on member demographics, conditions, and past behaviors. If you’re tailoring the resources shared with members based on their conditions and needs, it will help ensure they feel that your services and support feel comprehensive and address their specific needs, helping to improve your star rating.
3. Improve Member Experience Through Communication
Tied to: Rating of Health Plan, Rating of Healthcare Quality, HEDIS and HOS Scores
Send regular, friendly, and clear updates about available resources and services, plan benefits, or changes. Proactive engagement improves ratings on CAHPS measures and helps improve overall HOS and HEDIS ratings by ensuring members feel like their plan is proactively providing the information they’re looking for, have easy access to the care they need and are satisfied with the services they are receiving.
Importantly, do not rely solely on email. To ensure the greatest level of awareness and engagement, use phone, text (SMS), email, and mailed campaigns to reach members in the format they’re most likely to engage with. Ensure your member navigation platform tailors recommendations based on member profiles, conditions, and past behavior. If you’re tailoring the resources shared with members based on their conditions and needs, it will help ensure they feel that your services and resources are comprehensive and address their specific needs.
4. Encourage Consistent Engagement
Tied to: All CAHPS Measures, HEDIS and HOS Score Improvement
Member engagement is a foundational driver of both perceived care quality and actual health outcomes, two pillars of the Medicare Star Ratings system. Measures collected through HOS, CAHPS, and survey-based HEDIS rely heavily on members’ reflections of their experiences and outcomes over time. Engaged members are more likely to report higher satisfaction with their care and plan (CAHPS), show improvement or maintenance of physical and mental health (HOS), and recall and acknowledge proactive communication from their providers (HEDIS-HOS).
To build and maintain engagement, MAOs should focus on ongoing, multi-channel, personalized touchpoints that reinforce support and accessibility throughout the member journey. Strategies include:
- Providing timely, relevant health education via email, SMS, phone and direct mail to empower members with a strong understanding of what is available to them, and easy access to all levels of services and resources to help manage their health.
- Using digital tools for regular check-ins (e.g., symptom trackers, mental health assessments, text-based surveys) to help members monitor and better understand their mental health and access the services or resources that are most appropriate for their needs.
- Empower network primary care providers with the knowledge and tools to direct patients to additional services and supports outside of their clinic appointments.
- Offering self-guided tools and care navigation to help members navigate available resources and services and understand the value of preventive action. Additionally, leverage care coordinators that can proactively reach out to members identified as at-risk.
- Building a culturally aware and accessible communications plan to ensure all members feel well supported with the resources, services and education available to them, particularly those with chronic conditions or marginalized populations.
- Celebrate small wins through your member facing tools (eg. congratulatory message after completing an assessment or accessing a resource) to encourage proactive health engagement, reinforce positive behaviors and strengthen member satisfaction.
5. Personalize by Member Segment
Tied to: HEI, All CAHPS Measures, Especially Rating of Health Plan
Leverage segmentation by condition, usage, or digital comfort level (based on past behaviors) to personalize outreach. For example, for high-need members, surface mental health or chronic care resources specific to their conditions, and serve newly enrolled members a guided benefit orientation or series of emails. Matching your communications to the unique context of your members will increase relevance and trust.
6. Proactively Flag At-Risk Patients and Close Gaps in Care
Tied to: HEI, All CAHPS Measures and HOS Score Improvement
Members who are already experiencing health challenges or functional decline are more likely to report negative experiences if their needs go unmet or if deterioration is not prevented. Proactively identifying these individuals before issues escalate allows health plans and providers to intervene early, reduce avoidable hospitalizations, and improve overall satisfaction, all of which are key drivers of Star Ratings performance. Here are some strategies to do so effectively:
- Leverage predictive analytics and utilization data to identify members at higher risk of worsening physical or mental health. These may include individuals with declining patient-reported outcomes (e.g. from HOS or in-platform screenings), recent hospitalizations or multiple chronic conditions.
- Integrate social determinants of health (SDoH) into risk models to better understand and address barriers to care, such as transportation, housing insecurity, or food access.
- Automate alerts and care management workflows that notify care teams when a member is flagged as at-risk, enabling timely outreach, proactive navigation support, care plan adjustments, or referrals to appropriate services.
7. Tailor Feedback as a Proxy for Medicare Survey Scoring
Tied to: All CAHPS Measures
Embed smart feedback tools into your member platform to ask high-weight proxy questions that reflect key CAHPS items, tailored to the specific services members are accessing. This allows real-time monitoring and proactive course correction, empowering you to improve member satisfaction and experience before surveys are circulated (more on this shortly), and gives you a strong proxy for how satisfied your members are.
8. Proactively Address Member FAQs to Remove Barriers
Tied to: Getting Needed Care, Customer Service, Rating of Health Plan
One of the most effective ways to reduce friction and increase member satisfaction is by answering the most commonly asked questions, both in your communications and in a centralized resource hub. When members struggle to find basic information, they often delay care, feel unsupported, or report negative experiences.
Build FAQ-driven content into your emails, SMS, mailed guides, and online portals. These should be searchable where possible, clear, and aligned to the way members phrase their needs.
Examples of high-impact member FAQs to address:
- “How do I find services or benefits that I am not using that could help me stay healthy?”
- “Does my plan cover mental health therapy or counseling?”
- “What tools are available to help me get active and track my progress?”
- “Are there any wellness programs included in my plan?”
- “Can I talk to a nurse or doctor about bladder issues without an in-person visit?”
- “Where can I find resources on how to reduce the risk of falling for myself or a loved one?”
- “Can someone help coordinate my care between different providers?”
- “What mental health check-ins or screenings are covered by my plan?”
- “Where can I find information about my coverage in my preferred language?
Proactively answering these questions, and others like them, will help improve access, enhance member trust, and boost performance on CAHPS measures like “Getting Needed Care” and “Rating of Health Plan”.
Leveraging Population Health Platforms to Improve Star Ratings
The strategies outlined above aren’t theoretical, they’re already being brought to life by the Medicare Advantage plans we support. Through our Population Health Platform, we’re helping health plans not only close performance gaps but also create more personalized, intuitive member experiences that directly impact CAHPS, HEDIS, HOS, HEI and overall Star Ratings. Here’s how our platform is making it happen:
Comprehensive Resources: Each hub collates and integrates all available resources and services provided by an MAO, ensuring that members know exactly where to go to find the support they need. The platform simplifies the member journey, effectively supporting members to easily find and access services, have their FAQ’s answered, and better understand their overall wellness.
Personalized Resource Recommendations: Automatically customizes recommended resources specific to each member’s needs, ensuring they see what’s most relevant to them based on their demographics, goals and assessment results ultimately helping improve member satisfaction and outcomes.
Multi-Channel Outreach Enablement: Supports integrated phone, SMS, email, and physical mail campaigns, ensuring members are reached where they’re most likely to engage, improving perception of support even if they don’t immediately take action. With multi-channel, tailored outreach MAOs can support ongoing member engagement, improving overall ratings and driving long-lasting health outcomes.
Enhanced Retention: Drive long-lasting member engagement with built-in Measurement-based Care assessments. Our Population Health Platform has an average 30-day user retention rate of 43%, compared to an industry average of just 3%. This is based on aggregate data from 2021-2025 and reflects the impact of personalized outreach, multi-channel delivery, and embedded assessments. 93% of users return to complete their self-assessment and access their results and insights. This high engagement correlates with improved self-reported health outcomes, based on the number of assessments completed and tracked symptom improvement over time. These outcomes align with HOS and HEDIS effectiveness measures that directly influence Star Ratings.
Risk Stratification: The system leverages AI and predictive analytics to identify high-risk and underserved members, enabling targeted campaigns, early intervention, and prioritized support that improves access and care experience for those most at-risk. Plan All-Cause Readmissions is one of the most heavily weighted CMS measures at 3x in the 2025 Star Ratings. By identifying members at risk of rehospitalization through predictive analytics, our platform triggers case management workflows and outreach at critical moments. Care teams are notified early, enabling them to proactively intervene, adjust care plans, and proactively support the member at any high-risk, high-acuity moment. This reduces preventable readmissions and supports better outcomes, helping plans avoid score penalties and maximize bonus potential.
Performance Monitoring: Tracks usage, satisfaction, and impact, so you can see which resources and services are being used, which are having a positive impact on member outcomes, and where resource or service gaps exist to inform improvement and innovation–all of which will help to improve clinical outcomes and member sentiment. Our platform also incorporates validated SDoH assessments (eg.PRAPARE/PHED), enabling plans to stratify outcomes by social risk and satisfy HEI reporting requirements.
Proxy Satisfaction Surveys & In-Platform Feedback: Embedded micro-surveys and popup prompts offer ongoing insight into satisfaction, serving as real-time proxies for CAHPS and HEDIS scores; helping your team understand which user actions are correlated to enhanced member experiences.
Data Integration: Creates a unified view of each member’s health profile, service use, and engagement patterns, which is the foundation for proactive care management, personalized support, and seamless navigation throughout your services and resources.
Single-Sign On and Integration: Ensure seamless member navigation by connecting all services and resources through one system with single-sign on and EHR integration. Enable the automatic syncing of client information across systems, automatically set and schedule assessments, and connect users to all your services and resources with the ability to schedule appointments into your direct care options.
Together, these capabilities make it easier for your members to know what resources are available to them and where to access the support they need. They also make it easy for MA leaders to understand what’s working, what’s not, and continuously iterate to boost your performance across the board.
Boost Your Star Rating with Population Health
Improving your CMS Star Rating isn’t about chasing metrics, it’s about centering your strategy on what members actually value and what can directly impact CMS Star Ratings question responses. By addressing high-weight questions with precision and leveraging a comprehensive data-driven digital front door to operationalize your plan, you can meaningfully elevate both member satisfaction, financial performance, and deliver more impactful, member-centered care.
Ready to lift your Star Rating? Schedule a call today to explore how our population health platform can help enhance your member experience and CMS Star Ratings.