There’s been a growing focus within behavioral healthcare on developing integrated care models that can address the often co-existing or complex mental and physical health issues experienced by individuals. By bringing together multidisciplinary care teams, individuals receive more comprehensive assessment (both upfront and throughout care), experience improved outcomes and the overall cost of healthcare delivery reduces as a result. Keep reading to learn more about the Collaborative Care model, its foundational elements, and insights around implementation.
The Collaborative Care Model
The Collaborative Care Model (CoCM) is a type of integrated care designed to better support individuals struggling with one or more mental health conditions. When a common mental health condition like depression or anxiety becomes chronic or persistent, the collaborative care model will introduce more regular and frequent follow-up appointments with a team of primary care providers and behavioral health professionals that work together to support all of the individuals presenting concerns. There’s also an added requirement to track outcomes, incorporate Measurement-Based Care practices, and customize treatment according to the unique needs of each individual.
The practice was originally developed out of the University of Washington and has since been heavily researched and tested in 80+ randomized controlled trials. It surpasses many other integrated care models in the evidence supporting its effectiveness. The research shows that Collaborative Care models are more effective than usual care at improving outcomes, functioning, increasing client and provider satisfaction, and reducing overall healthcare costs.
The CoCM team Structure

Collaborative care models take the structure of the care team from two people (the Primary Care Provider and the patient) to four. Primary Care Providers (PCPs) don’t typically have enough time allotted to deep dive on the mental health concerns of the client. With the CoCM model, there are two additional team members to support every individual in care:
- First addition is the Behavioral Health Care Manager (BHCM), who is responsible for coordinating the care team, ensuring effective communication, and assigning tasks and next steps to the team of providers.
- Second addition is the Psychiatric Consultant, who will support both the Primary Care Provider and the BHCM with diagnosis, treatment planning and treatment changes, whenever needed.
The 5 Core Components of CoCM
There are 5 core elements to the Collaborative Care model which are key to ensuring a successful implementation:
1. Patient-Centered Team Care
The key to the right care team is one that can collaborate on care plans that are designed around the clients personal treatment goals. Centering the clients voice in treatment and ensuring they can easily communicate their needs to their providers will promote higher engagement in the overall care process. It’s also important that the client can be treated by their care team within one location (or virtually) and that there is a system for information sharing between providers that eliminates duplicate assessments and improves treatment alignment.
2. Population-Based Care
By actively monitoring people in care grouped by similar population subsets and symptoms, care teams can quickly identify when someone is not improving and treatment change is needed. The team’s mental health specialist can then address concerns specific to the clients they serve, rather than using a one size fits all approach.
3. Measurement-Based Treatment to Target
In order to easily recognize necessary changes, treatment plans should be personalized based on the persons individual goals and clinical outcomes. Routine, evidence-based measurement tools are used to monitor progress, inform collaborative discussions between the person in care and providers, and inform any necessary changes to the treatment plan.
4. Evidence-Based Care
Treatments offered to client are evidence-based, meaning there is substantial research supporting the effectiveness of the methods or approached used.
5. Accountable Care
Under Collaborative Care models, providers are reimbursed based on quality of care and clinical outcomes, rather than the number of sessions or treatments provided (aligned with the approach of Value-Based-Care).
The role of Measurement-Based Care
What’s clear in the fundamental components of Collaborative Care, is that it must be rooted in an effective measurement process. Using an evidence-based approach to measurement, like Measurement-Based Care, allows care teams to incorporate the routine collection of patient-reported outcome measures throughout treatment. The data collected is then assessed and used to inform treatment planning, clinical decision making, and to foster collaborative discussions with clients. MBC empowers data-driven decision-making to help assess the unique challenges of people in care and design treatment plans that meet their needs.
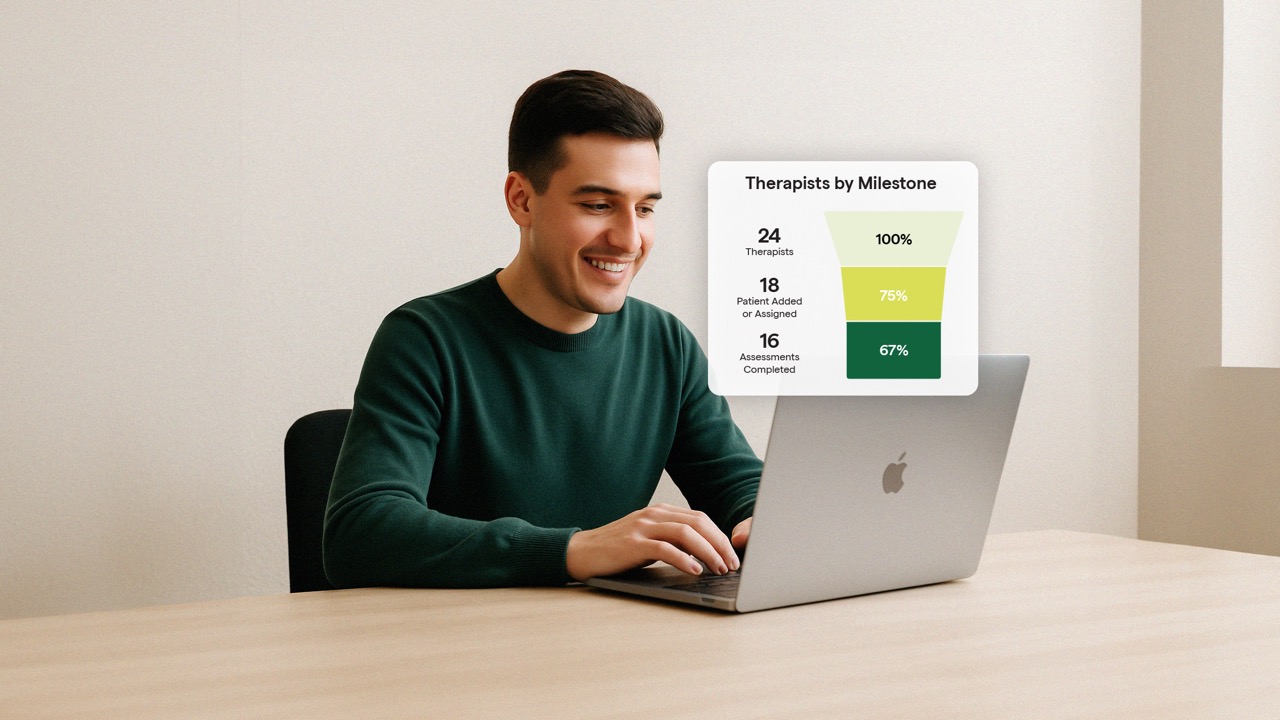
To illustrate this connection, let’s walk through what collaborative care facilitated by an MBC system like Greenspace looks like in practice.
- To start, the Primary Care Provider would have a set group of assessments automatically assigned and delivered to any person who is seeking treatment for mental health concerns, tailored to their presenting issues. The results are visualized in a dashboard and can be filtered by client, location, program, etc— meaning the PCP can quickly identify people in care that may need the extra support of a collaborative care team. High-risk patients are automatically flagged based on assessment scores, so they can ensure no one falls through the cracks. The PCP can create session notes that will be shared across the provider team and can view assessment results prior to treatment sessions.
- As the team’s coordinator, the Behavioral Health Care Manager can view the patient’s dashboard, add assessments that address the unique concerns of the individual, and set a schedule for them to be remotely delivered to the client. If the BHCM is delivering psychotherapy as part of treatment, they’re able to examine assessment results with the patient in session. The BHCM can then work with the patient and get curious about what their data says, how they’re feeling, and how they’re responding to care.
- Since the Psychiatric Consultant typically doesn’t directly treat patients or prescribe medication, access to quick, visualized insights derived from regular patient-reported measures is extremely important. With all this contextual information at their fingertips, they can stay in the loop on the patients symptoms and needs, identify when they’re not improving, and offer treatment modifications whenever necessary
- The patient can be confident that everyone on their care team is aligned and have a deep understanding of their symptoms, experiences, and goals. By offering patients access to their own results dashboard, they can monitor their own symptoms and cultivate a deeper understanding of their emotions, triggers, and needs. Having access to their own data dashboard helps the patient build a shared language with their PCP and feel empowered to communicate their experiences with their providers.
- Finally, all providers on the care team have the outcome data needed to be reimbursed based on the quality of care they delivered, rather than number of sessions. The team also has rich insights from each person in care and the overall population they serve, which they can use to inform treatment innovation and improvement moving forward.
To learn more about how MBC and Greenspace can support your collaborative care team, visit greenspacehealth.com to schedule a call with one of our implementation experts today.