The Need for High-Quality Behavioral Health Care and Upstream Preventative Services
A recent Milliman research study, conducted by the Mental Health Treatment and Research Institute, explores the impact of behavioral health conditions on overall healthcare spending. The study examines data from 21 million commercially insured Americans, focusing on the prevalence and costs associated with mental health and substance use disorders (SUDs) and their contribution to total healthcare spending.
The dataset reveals an alarming trend: individuals with behavioral health conditions make up a disproportionate percentage of physical healthcare costs, yet there is minimal spending on actual behavioral health services for those individuals. This highlights an urgent need for improved behavioral health service access, particularly upstream and preventative care, in order to prevent acute challenges that impact people’s quality of life and lead to drastically increased physical healthcare costs.
Key Findings
The study’s findings highlight the severe cost impact of untreated or minimally treated behavioral health conditions:
- High-cost concentration: When examining healthcare costs across the study group, the top 10%, highest-cost individuals accounted for about 70% of total healthcare spending. On average, this group incurred 21 times more healthcare costs annually than the remaining 90% of the study population.
- The cost of behavioral health conditions: Among those in the 10% high-cost group, more than half (57%) had co-existing behavioral health conditions. This small behavioral health group accounted for 44% of total healthcare costs, despite being only 5.7% of the total population. However, behavioral health services constituted a minor fraction of their spending, which indicates a lack of appropriate or sufficient care for behavioral issues.
- Minimal spending on behavioral health treatment: Despite the clear impact of behavioral health challenges on healthcare costs, half of the high-cost behavioral health group had less than $95 allocated to behavioral health treatment annually (despite their average overall healthcare spending of $45,782).
This pattern of limited investment in behavioral health services suggests an overlooked opportunity to drastically reduce care costs through enhanced behavioral health service access.
The Need for High-Quality Behavioral Health Care and Upstream Preventative Services
These findings illustrate the need for proactive behavioral health interventions to alleviate the overall healthcare burden and address a major gap in our behavioral healthcare system. With an average 11-year delay between symptom onset and the initiation of treatment for behavioral health issues, timely access to care is far from ideal. During this period, unmanaged symptoms lead to worsening mental health and physical comorbidities, which drive up healthcare service burden and costs. Timely access to mental health services reduces the need for more acute—and costly—interventions, and reduces the physical health costs associated with behavioral health challenges.
Where Do We Go Next? A Population Health Solution
It’s evident that as an industry, we need to invest in early intervention and preventative care models. Prioritizing proactive identification and intervention of behavioral health challenges would meaningfully reduce the high physical healthcare costs associated with them, and increase the populations overall quality of life.
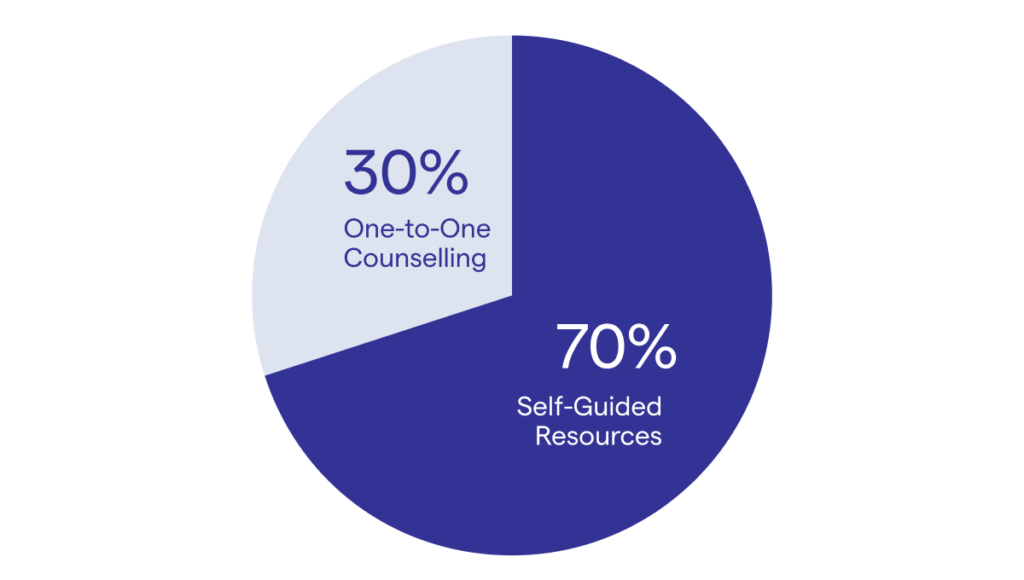
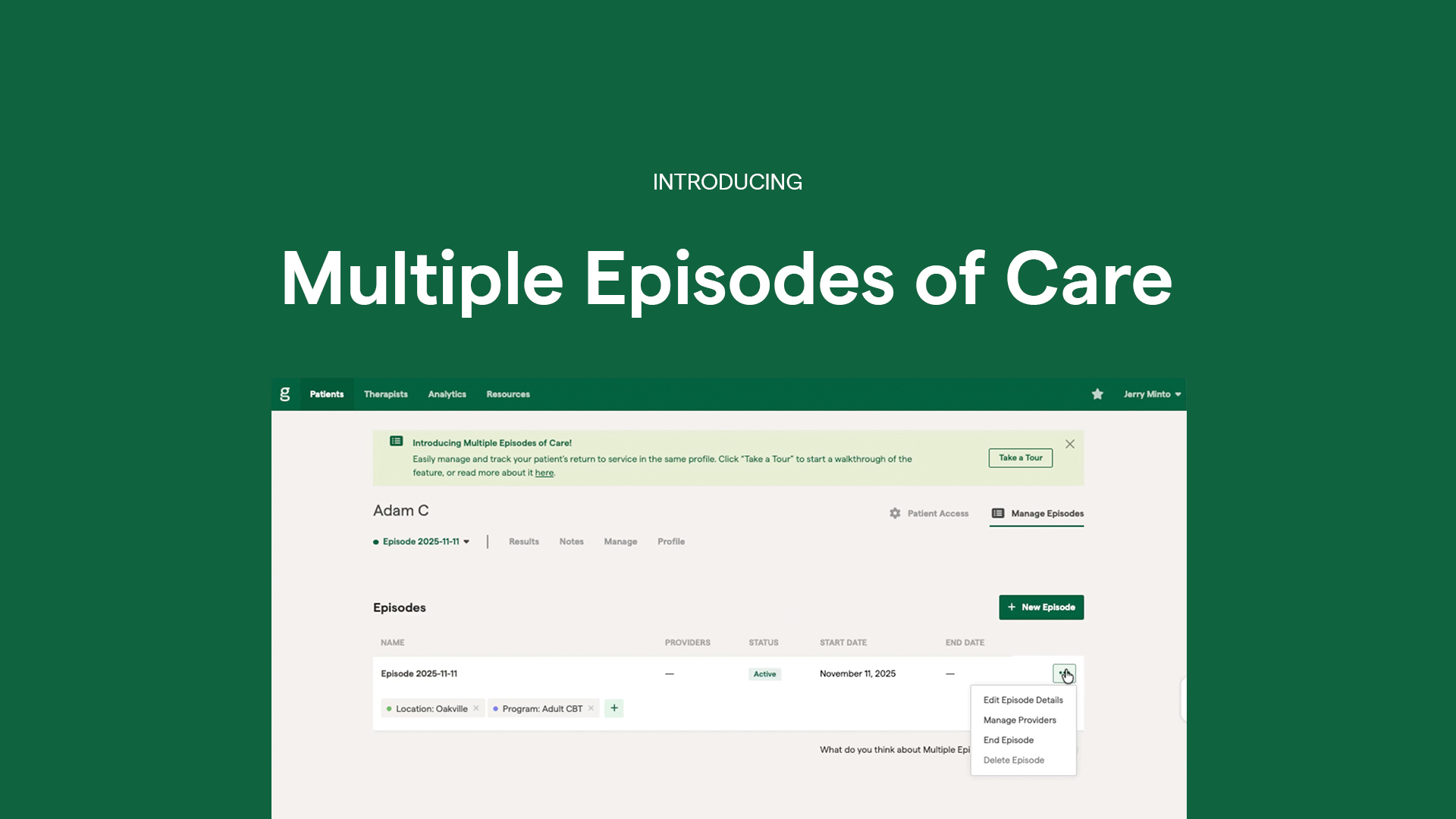
As an example, our Population Health Hubs were designed to provide a proactive solution to this challenge by acting as a digital-front-door for individuals within any health system to easily find and access the behavioral health resources available to them. User data from our Population Health Hubs reveals that, when provided the choice, over 70% of users opt to begin with low cost, self-guided resources before seeking 1:1 care.
Grounded in the principles of Measurement-Based Care (MBC), individuals are empowered to monitor their mental health through bi-weekly self-assessments. This continuous tracking allows individuals to better understand their own mental health, recognize periods of increased struggles, and more actively participate in their own wellness journey. Data shows that this approach significantly increases engagement and retention in resources and services, and that individuals who consistently complete self-assessments report greater symptom improvement. With a stronger understanding of their own mental health, people can engage in resources and care that are most appropriate for their challenges leading to improved outcomes, alleviating demand on high-cost services, and providing more timely access to acute care for those most in need.
At the system-level, insights derived from aggregate usage and outcome data empower health systems to understand population-wide and demographic-specific needs, evaluate the effectiveness of available resources, and identify and respond to resource and service gaps. This Population Health model is a scalable, preventative approach to behavioral healthcare that improves access, enhances mental health outcomes, reduces costs and empowers individuals and organizations to more effectively manage behavioral health challenges.
Greenspace's Population Health Hubs
Interested in learning more about how Greenspace can simplify and enhance your measurement practice?
Book a CallBottom Line
There is a very real fiscal and human cost of neglecting behavioral health conditions. By investing in preventative and integrated behavioral healthcare options, we can address a critical behavioral health need, reduce total healthcare costs, and ultimately improve the quality of life across any population. It’s time for the healthcare industry to prioritize behavioral health as an essential component of holistic health and wellbeing, and we will all be better off for it.