Number of Participating Clinicians: ~2,000
Number of Participating Clients: ~30,000
Population Served: Canadians dealing with mental health and substance abuse issues
Program Type: Inpatient & Outpatient Mental Health & Addictions Programs
Org type: Private
Greenspace Platform: Measurement-Based Care
Key Assessments: PHQ-9, GAD-7
As the Canadian leader in mental health and addictions services, Homewood Health is deeply dedicated to delivering outstanding outcomes for every individual they serve. They offer a comprehensive continuum of care, with services ranging from organizational training programs and employee assistance programs to direct mental health services, as well as specialized expertise in mental health assessments, return to work assistance, recovery management, and family support.
Homewood has been a pioneer in Measurement-Based Care (MBC) and partnered with Greenspace in 2018 to continue their journey. Through MBC, Homewood has enhanced the standard of care available to the thousands of individuals they support throughout Canada. Their implementation has been iterative, with their workflow and strategy adapting each year based on clinical outcome data, engagement metrics, and insights they’ve collected across their services. The partnership with Greenspace has allowed Homewood to present key clinical measures in an easily digestible way, allowing clients and clinicians to engage with the information to inform their care path.
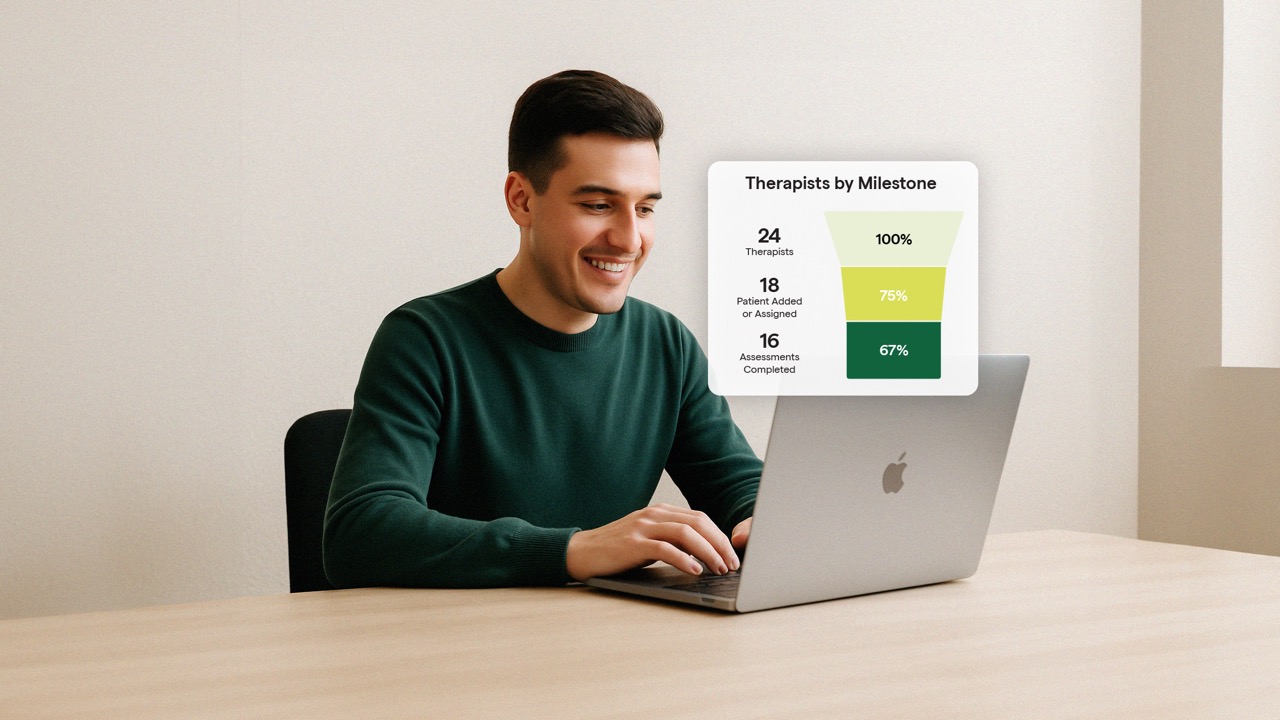
Today, Homewood has over 30,000 participating clients and 2,000 participating clinicians actively using Greenspace across all their inpatient and outpatient services, and their outcomes are exceptional. Because they’ve created an iterative MBC process that adapts and works to improve care in response to their data, Homewood has seen improved clinical outcomes and importantly, improved engagement between clients and clinicians, demonstrated by an average therapeutic alliance score of 82%.
During our educational session with Homewood’s Director of Research and Outcomes, Shannon Remers, she shared some of the key factors that have contributed to the organization’s overall success with MBC. We’ve collected the main implementation insights that Homewood has leveraged to progress towards the clinical outcomes they have today. Some of these factors were embedded in their implementation, while others were the result of continuous learning and adaptations along the way.
Keep reading to discover Homewood’s tips to success with MBC:
1. Choose measures that matter to your stakeholders
Determining which measures to use across clients and programs can be intimidating for organizations getting started with MBC. At Greenspace, it’s one of the questions we are asked about most during the implementation process. The selection of measures used to assess clinical outcomes from organization to organization often differ widely, and will depend on a few critical factors: what types of populations you’re treating (age range, background, race, income, etc.), what types of services you offer, what symptoms your clients are navigating, and what reporting requirements you have to meet.
Homewood Health uses a variety of symptom measures, functional measures, as well as quality of life measures. Their most commonly used assessments include the PHQ-9 for depression and GAD-7 for anxiety. When selecting their measures, a critical step for Homewood was hosting focus groups with clinicians, clients, researchers (including research scientists from the Homewood Research Institute), and government/political stakeholders in order to define what would best indicate success in treatment and what would provide the most value to their
stakeholders, with a particular focus on clinical value for clients and clinicians and could inform quality improvement across the organization.
Shannon shares an example of how this influenced their assessment library, where they chose to add and leverage a hopefulness measure after many discussions where clients identified hope to be an important measure of success for them in care:
2. Adapt MBC to your specific programs
As a national mental health services provider, Homewood Health offers a variety of service options and programming across Canada—all of which operate in unique ways. They recognized early that being a leader in Measurement Based Care would require a comprehensive and enduring commitment across the organization. As they expanded their implementation of MBC across various services, they focused on ensuring their implementation was flexible and that their clinical leaders were empowered with the ability to adapt MBC to their
programs’ unique needs.
For example, in many of their inpatient programs, Homewood determined that it would be beneficial to host group sessions to introduce clients to MBC to ensure they understood the value of MBC to their care and were comfortable completing assessments. In these sessions, they carve out dedicated time for clients to complete assessments and ensure it is in a supportive environment where someone is present if they have questions or are uncomfortable by the content of any assessment. At the beginning of these sessions, they reiterate the value and goals associated with assessment completion, which has helped to motivate and engage clients.
As they move through treatment, clients have the option of remaining in the group if they choose or, once comfortable, they can begin to complete assessments on their own time.
With any implementation, it’s important to take stock of the data and outcome needs of your specific services and current operational processes to ensure that MBC flexes to your workflow. This will help create a seamless experience for both providers and clients as they move through treatment.
3. The impact of MBC centers around integrating outcomes into your regular clinical discussions
Bringing client outcomes into session and using them as a springboard for collaborative discussions with your clients is how MBC becomes most impactful. But how do you ensure that clinicians and clients see the value of MBC and feel comfortable integrating it into practice? Homewood’s recommendation is to start simple.
To help drive engagement from clinicians and ensure they saw the immense value that MBC would bring to their treatment process and the importance of orientation and ongoing training to this approach. Homewood encouraged their clinicians to start small and hone in on one or two assessments that they believe would provide helpful insights to guide the first 2-5 minutes of their sessions. It’s important to help clinicians get comfortable being curious about their clients assessment scores and find a simple way to leverage MBC to enhance their care and see how easily it can be incorporated into their clinical process. Once they’ve established a process and have integrated it into sessions, it becomes easy for both clients and clinicians to notice trends or meaningful changes in their outcomes and leverage those to inform treatment discussions and adjustments.
When MBC is integrated into treatment, engagement from clients will follow. Shannon shares that during their initial introduction, many clients immediately see the value that MBC provides. But, for those that do not, the key has been to continually integrate the results into sessions so that clients can gain an understanding of how their results will inform discussions and act as an additional signal to their provider when things were or were not progressing in treatment, so they could explore potential adjustments.
Shannon shared a story from one of their inpatient substance use programs, where a client was not engaged with their assessments and was contemplating leaving the program early. By diving into that client’s results, she was able to identify how to adjust their treatment to better support them, which was key to them completing the program and achieving recovery.
4. Where possible, integrate MBC into your current technology and processes
Embedding MBC into existing processes and integrating it with a clinic’s current workflow and technology is a key component to any successful implementation. In Homewood’s case, they have administrators within each of their service offerings whose key responsibility is to onboard and engage clients into their programs. Another example would be integrating MBC with your EHR, which allows for the EHR to remain as the sole source of truth for all client information, helps ensure there is no extra burden of measurement on providers, and that MBC is deeply
integrated into existing processes.
Ultimately, the adoption of MBC is much simpler when it can be embedded in existing processes and technology. Doing so will improve the experience for clinicians and administrators, eliminating extra (and often removing existing) administrative burden—which in turn allows them to spend more time ensuring a positive experience for clients and improving their outcomes in care.
Final Thoughts
Though every implementation will look different based on the unique needs of specific organizations, the services they offer and population they support, the insights from Homewood’s very successful MBC implementation can help guide how your team approaches MBC. Ultimately, it’s about making MBC work for your staff, clients, and workflow in order to create a seamless experience and derive the most value from the outcome data you’re collecting and the discussions clinicians are having with their clients.
It’s been a pleasure working with Homewood throughout the years and watching how their implementation has continually evolved. We want to thank Shannon for sharing her insights with us and all behavioural health leaders and providers, as they work to implement MBC to significantly enhance their standard of care.
If you’d like to discuss how to implement MBC at your organization and learn how Greenspace can support your measurement goals, please schedule a call or reach out anytime at info@greenspacehealth.com.