New Standards for CARF Accreditation: The Impact of Measurement-Based Care
This article features clips from ‘Measurement-Based Care & CARF Accreditation: Driving Quality Through Measurable Outcomes‘, an educational webinar hosted by Greenspace Health.
The Commission on Accreditation of Rehabilitation Facilities (CARF) recently released its 2025 Behavioral Health Standards Manual, which introduces a new requirement for organizations to incorporate a procedure for Measurement-Informed Care (MIC)—also commonly known as Measurement-Based Care (MBC). While the terminology used across the industry may vary, both MIC and MBC are used interchangeably to describe the clinical practice of using standardized assessments to routinely track a person’s symptoms and progress throughout care. The outcome data is then used to inform clinical decision-making and foster collaborative discussions between providers and their clients.
In the following clip, Michael Johnson, Senior Managing Director of Behavioral Health at CARF, shares why the new standard for MBC / MIC reinforces CARF’s commitment to individualized, person-centered and high-quality care.
In order for CARF accredited organizations to understand the importance of CARF’s updated accreditation requirements and how to prepare for them, this article will explore what the requirements involve, how they impact clinical care, CARF’s guidance on successful adoption, and how organizations can leverage Greenspace to enhance treatment outcomes, meaningfully improve care quality and align with CARF’s MIC / MBC requirements.
Behind CARF’s 2025 Standards for Measurement-Based Care (MBC / MIC)
MBC is revolutionizing behavioral healthcare by equipping clinicians with timely, objective data to guide clinical decisions and improve treatment outcomes. By routinely administering standardized assessments, MBC enables providers to monitor symptom changes, detect when clients are not improving, and proactively adjust treatment plans based on their clients’ experiences and clinical outcomes. The addition of MBC to CARF standards comes alongside a widespread increase in the adoption and industry-wide recognition of its role in enhancing care quality, preparing for evolving value-based payment models and meeting accreditation requirements. With other accrediting bodies like the Joint Commission already recognizing MBC as a foundational component of high quality, evidence-based care, organizations are increasingly motivated to adopt MBC into their practice.
Why CARF Introduced a New Standard for Measurement-Based Care
With thousands of CARF-accredited organizations across behavioral health and human services, the organization plays a key role in setting the direction for care quality and accountability. By introducing MIC / MBC into its requirements, CARF aims to accelerate the use of data-driven insights to improve care quality, strengthen service delivery, and increase access to timely, effective care. In the following clip, Michael Johnson shares the reasoning behind CARF introducing a new standard for MIC / MBC.
The Industry-Wide Benefits of MBC: From Client Care to Behavioral Health System Quality
MBC creates measurable value for clients, empowers providers, and strengthens organizational performance. For clients, the use of outcome measures fosters engagement and empowerment by providing clear insight into their symptoms and progress to help them better understand their mental health, encouraging more active participation in treatment decisions and improved collaborative discussions and decision making with their provider. Providers are able to access insights specific to each individual client to better understand how they are doing throughout care, better tailor care to their specific challenges, easily identify off-track clients and proactively intervene; all leading to more client-centered and effective care. With MBC, organizations are empowered to leverage their clinical data to assess the effectiveness of programs, drive continuous quality improvement, improve operational efficiency and easily share the impact of their services with funders, payors and accreditors.
In this clip, Michael Johnson elaborates on the value of MBC, explaining how the CARF standards are designed to drive population-level improvements, ultimately enhancing care quality and operational efficiency across the entire behavioral healthcare system.
MBC’s Role in Driving Value-Based Care
MBC also plays a critical role in advancing behavioral health parity and supporting value-based care (VBC) models. By systematically capturing outcome data, organizations are empowered to clearly demonstrate the effectiveness of clinical interventions to payors and other funders. This transparency eases reporting processes, builds trust between service organizations and funders, empowers organizations to advocate for increased rates and new funding, and fosters equitable access to high-quality care. As Michael Johnson explains, MBC helps create a data-driven foundation that aligns service delivery with value, enabling organizations to demonstrate the meaningful impact their care provides.
CARF’s Requirements for Measurement-Based Care (MBC / MIC)
Standard 2.A.12, newly introduced in CARF’s 2025 Behavioral Health Standards Manual, requires organizations to develop a clear, written procedure for implementing MIC / MBC. Watch as Michael Johnson explains the requirements associated with the updated standards:
Organizations implementing MIC / MBC for CARF accreditation must develop a procedure that addresses the four areas described below:
- Identify the tools to be used: Organizations must select and clearly define the standardized assessment tools that will be used to meet the needs, goals, cultural and linguistic backgrounds, and reading levels of the individuals they support. Common examples of behavioral health assessment tools include, but are not limited to, the PHQ-9, GAD-7, DAST-10, and BR-WAI. When used consistently throughout care, these measures help monitor client symptoms over time, inform meaningful clinical discussions and treatment decisions, and ensure that care plans remain focused on the evolving goals, needs, and experiences of those being treated. There are hundreds of evidence-based assessments for clinical leaders and clinicians to choose from, what’s important is that the assessment tools used respond to the needs of the specific goals of each service line. To explore other evidence-based assessment tools, you can visit Greenspace’s Assessment Hub.
- Prescribe intervals for administration of the tools: Organizations must set clear guidelines for how frequently assessment tools are administered, tailored to each service line and individual’s condition and needs. Common intervals can include a baseline assessment before starting treatment, regular monitoring at specified intervals throughout treatment (Greenspace recommends assessments be assigned every two weeks, but individual measures will often have recommendations that have been validated by the authors), and as-needed assessments at critical transition points or when there are additional concerns about a person’s condition.
- Outline how results will be shared with individuals in care: A core aspect of MIC / MBC is sharing assessment results with the individuals receiving care. Having access to their own results and regularly reviewing results and discussing symptom changes helps clients understand the value of the measurement process on their care quality. Sharing results with clients also helps to enhance client engagement throughout care, increase treatment adherence, and improve clinical outcomes. CARF requires organizations to have a defined process for sharing assessment results with clients to increase transparency, accountability, and strengthen therapeutic alliance.
- Identify personnel training required: To support effective implementation, organizations must provide comprehensive training for clinical staff. This includes sharing the rationale for using MIC / MBC, guidance on administering and scoring assessment tools, and strategies to interpret and respond to results. When clinicians are well-informed on the benefits of MIC / MBC and genuinely engaged, they’re well-positioned to inspire the same level of curiosity and participation in their clients. That’s why it’s essential to support them with ongoing training, practical tools, supportive resources, and strong leadership support throughout implementation and day to day practice.
CARF’s Guidance on Implementing Measurement-Based Care (MBC / MIC)
Michael Johnson shares CARF’s recommendation for a collaborative approach to MBC implementation that involves all the key stakeholders in an organization, rather than a top-down mandate. Taking into consideration the various needs and challenges faced by clinical staff and other stakeholders, can help an organization align on their approach to implementation, clinical goals and target areas that MBC can help address.
There is also value behind an intentional, iterative process to sustainably incorporate a well thought-out MBC system into practice. Taking the time to evaluate the needs of the organization, its clinicians, and its clients can empower an effective MBC process that positively impacts client experiences and outcomes. Ultimately, Michael Johnson emphasizes the importance of having a well thought-out implementation plan to successfully adopt MBC into your organization and deliver higher quality care.
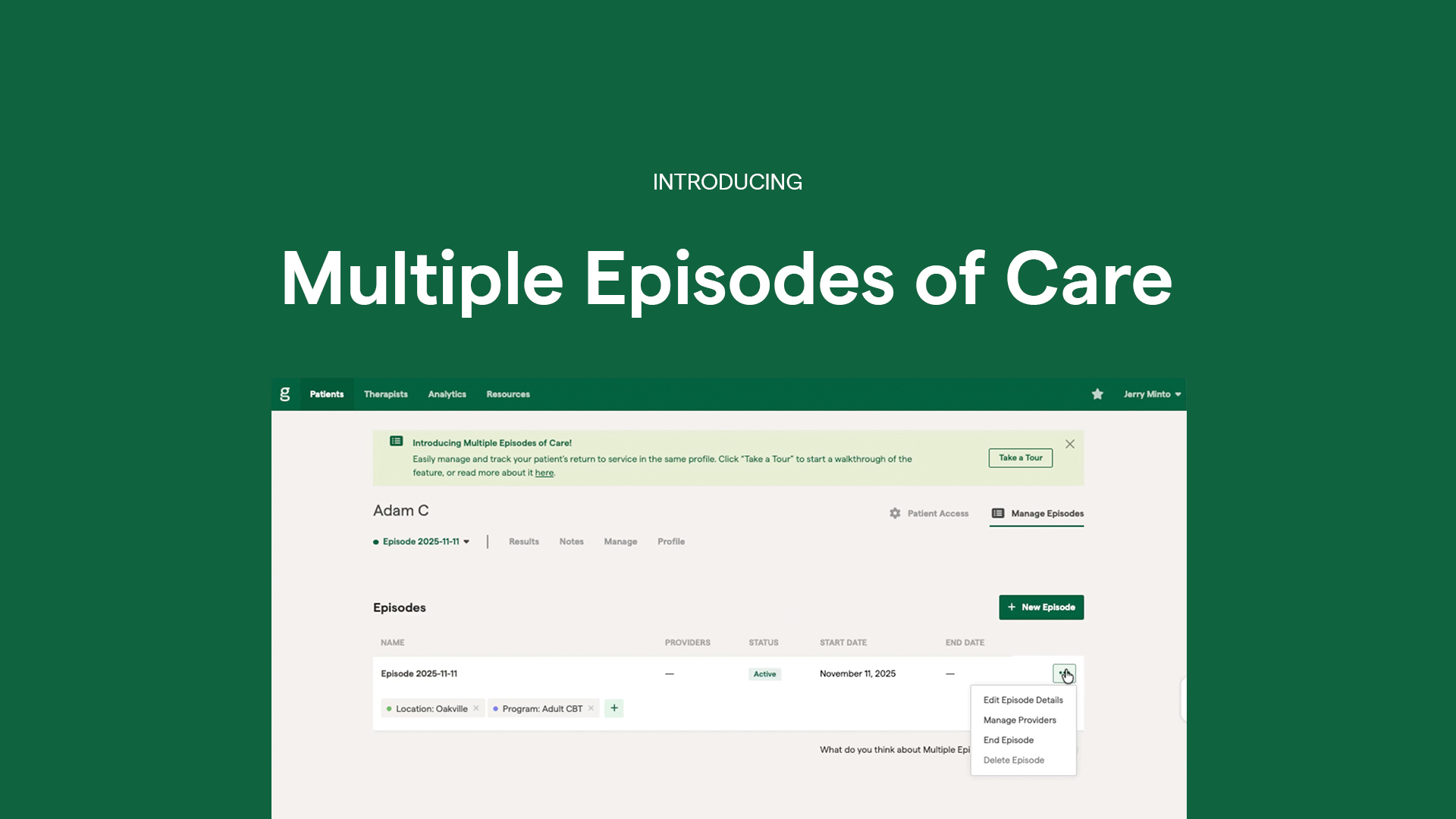
Greenspace has partnered with many CARF-accredited organizations, playing a key role in helping them achieve and sustain compliance with accreditation standards. Our Measurement-Based Care (MBC) platform offers a seamless, purpose-built solution for organizations dedicated to delivering high-quality care aligned with CARF’s behavioral health standards for progress and outcomes measurement.
Achieving CARF Accreditation with Greenspace Measurement-Based Care (MBC / MIC)
Here’s how Greenspace can support your organization in easily implementing each of the CARF requirements outlined above:
- Tools: Greenspace has over 400 evidence-based assessments available on our platform, with the flexibility to customize the measures used based on an individual’s presenting issues and symptoms, as well as the ability to add any additional assessments a clinic is looking for. The battery of assessments used can also be customized for each specific service line. Clients can complete assessments remotely (via SMS or email) and/or in person through a multilingual, user friendly platform. Our client-facing dashboard allows clients to complete assessments and reflect on their results in their preferred language. With over 3 million assessments completed to date, our clinical partners have achieved an average symptom improvement score of 49%.
- Assessment Frequency: Tailor the frequency of assessment delivery based on client needs or program requirements and goals. Clients can complete assessments at home via email or SMS, or in-person through our Kiosk tool before, during, or after sessions. Remote assessment settings, including frequency and timing, are fully configurable to align with your clients preferred delivery methods and schedule. Providers can adjust assessment frequency or add new measures throughout care based on clinical needs, ensuring flexibility as treatment evolves.
- Communicate Results: Client visibility is a core pillar of MIC / MBC, which means providing clients with access to their results, empowering them to better understand their symptoms and progress and take a more active role in their care process. This transparency supports more meaningful clinical conversations and collaborative decision-making. Evidence shows that empowering clients with visibility into their own results has a significant impact on clinical outcomes. Particularly with clients considered not-on-track, one study found that clients receiving regular feedback on their results saw twice the rate of clinically significant change (23% vs. 10%) compared to those who did not (Hawkins et al., 2004). Learn more about the impact of client visibility here.
- Training and Implementation: With over a decade of experience across hundreds of MBC implementations, we’ve refined our approach to provide comprehensive support and ensure a smooth, effective implementation of MBC across your organization—encompassing everything from service flow customization and assessment selection to clinician training and resources for client education and engagement. Having partnered with over 500 behavioral health organizations—ranging from small clinics, to large community clinics, hospitals and complex health systems—we’ve successfully supported MBC implementations across the full ecosystem of behavioral health services. Our dedicated Customer Success team and implementation experts are on hand to help you get started and support the development of an implementation plan that aligns with your clinical needs, drives continuous quality improvement, and meets CARF requirements.
Wrapping Up
MBC / MIC has been recognized as a core component of delivering high-quality, evidence-based behavioral health services by CARF and other accrediting bodies, including the Joint Commission. Its value lies in equipping clinicians with real-time data and insights to inform care decisions, track symptom changes, and tailor treatment based on each individual’s needs, ultimately driving meaningful improvements in clinical outcomes. An organizations first implementation of MBC can feel daunting but it doesn’t have to be, which is why we partner with organizations across North America to provide the technology, tools, and expertise that make MBC intuitive and effective, while fitting naturally into your team’s existing workflows. Here’s an encouraging clip from Michael Johnson, where he emphasizes the purpose of MBC being to improve care quality, and highlights that getting started is more important than focusing on perfection.
If you’re interested in learning more about implementing MBC to meet accreditation standards and improve treatment outcomes, schedule a call with an implementation expert or reach out anytime at info@greenspacehealth.com.