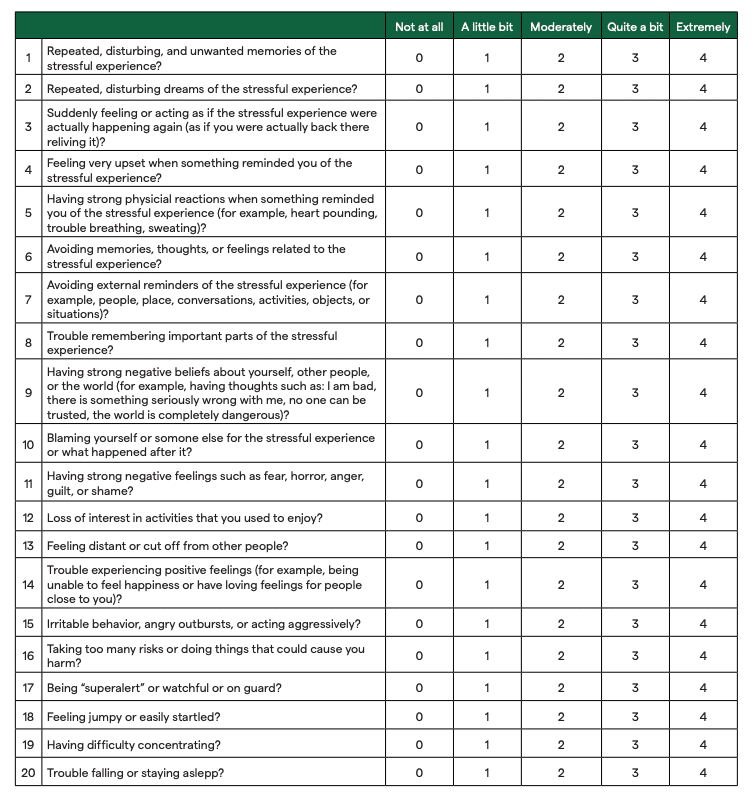
PTSD Checklist for DSM-V (PCL-5)
Recommended frequency: Every 4 weeks
Summary
The PTSD Checklist for DSM-V (PCL-5) is a self-report measure that assesses the 20 DSM-V symptoms of Post-Traumatic Stress Disorder (PTSD). The assessment has been validated for use with adults (18+), as a means of monitoring symptom change during treatment. The PCL-5 can also serve as a tool for screening individuals for PTSD or for making provisional diagnoses. Official PTSD diagnosis should be done through a structured clinical interview, but a provisional diagnosis with the PCL-5 can help indicate if an interview or external referral for diagnoses is needed.
We want to thank Dr. Michelle Bovin for sharing her expertise with us in the creation of this Assessment Guide. Dr. Bovin is a staff psychologist at the Behavioral Science Division of the National Center for PTSD and an Associate Professor of Psychiatry at Boston University Chobanian & Avedisian School of Medicine. She has worked to develop many evidence-based assessments and has led studies to validate several others, including the PTSD Checklist for DSM-5 (PCL-5). The views presented by Dr. Michelle Bovin are her own and do not represent those of any institution or the US government.
About the PCL-5 Measure
The PCL-5 is one of the most widely used self-report measures for PTSD. It’s well regarded for its ability to consistently demonstrate strong psychometric properties, such as internal consistency, test-retest reliability, and convergent and discriminant validity.
This version of the PCL was updated to correspond with the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), which includes adjustments to previously identified symptoms, as well as the addition of new symptoms included in the DSM-V. The assessment has a total of 20 questions that are each associated with an item under clusters B-E of PTSD diagnosis.
PCL-5 formats
There are three formats of the PCL-5 available. They each vary in the level of detail collected on Criterion A, which measures trauma exposure. The versions include:
- No Criterion A component.
- A brief Criterion A component
- Including the Life Events Checklist for DSM-5 (LEC-5) and extended Criterion A component.
Considerations to the PCL-5
The PCL-5 has a few limitations related to the fact that it’s a self-report measure:
- As mentioned, the PCL-5 should not be used to determine diagnostic status without the assistance of a clinical interview.
- The PCL-5 only offers information about the traumatic event if you use a version that has a Criterion A component.
- The PCL-5 does not provide information about the course of PTSD— meaning how it has or will progress— nor about the functional impairments caused by the PTSD.
It’s recommended that assessment scores be reviewed and discussed in session with the client. This can be a great opportunity to uncover information that may not have been captured within the assessment or to dive into particular responses where more information is needed, including when specific results may be surprising for the client or clinician.
When treating clients with PTSD, Dr. Michell Bovin shares that self-report measures like the PCL-5 are very powerful, “as they allow patients to check a box, rather than talk to someone— often a stranger— about what’s going on with them.”