Within Health: Enhancing Eating Disorder Treatment with Measurement-Based Care
- Implementing Measurement-Based Care in Practice
- Getting Started: Introducing MBC at Your Organization
- Getting Started: Supporting Clinicians and Staff Implementing MBC
- Getting Started: Selecting Outcome Measures for Eating Disorder Treatment
- MBC in Practice: Using Outcome Measures to Inform Eating Disorder Treatment
- MBC In Practice: Monitoring Co-occurring Conditions and Discharge Readiness
- MBC in Practice: Transitioning Out of Care with MBC
- Key Impacts of MBC in Eating Disorder Treatment at Within Health
Over the past 20 years, the percentage of the global population affected by eating disorders has more than doubled (Galmiche et al., 2019). With eating disorders having the second highest mortality rate among mental illnesses, there’s an urgent need for increased investment in high-quality, evidence-based, and accessible treatment. Within Health is a behavioral healthcare organization delivering comprehensive, virtual care for individuals across the U.S. affected by eating disorders. Their mission is to increase access, improve outcomes, and promote healing for tens of millions of Americans.
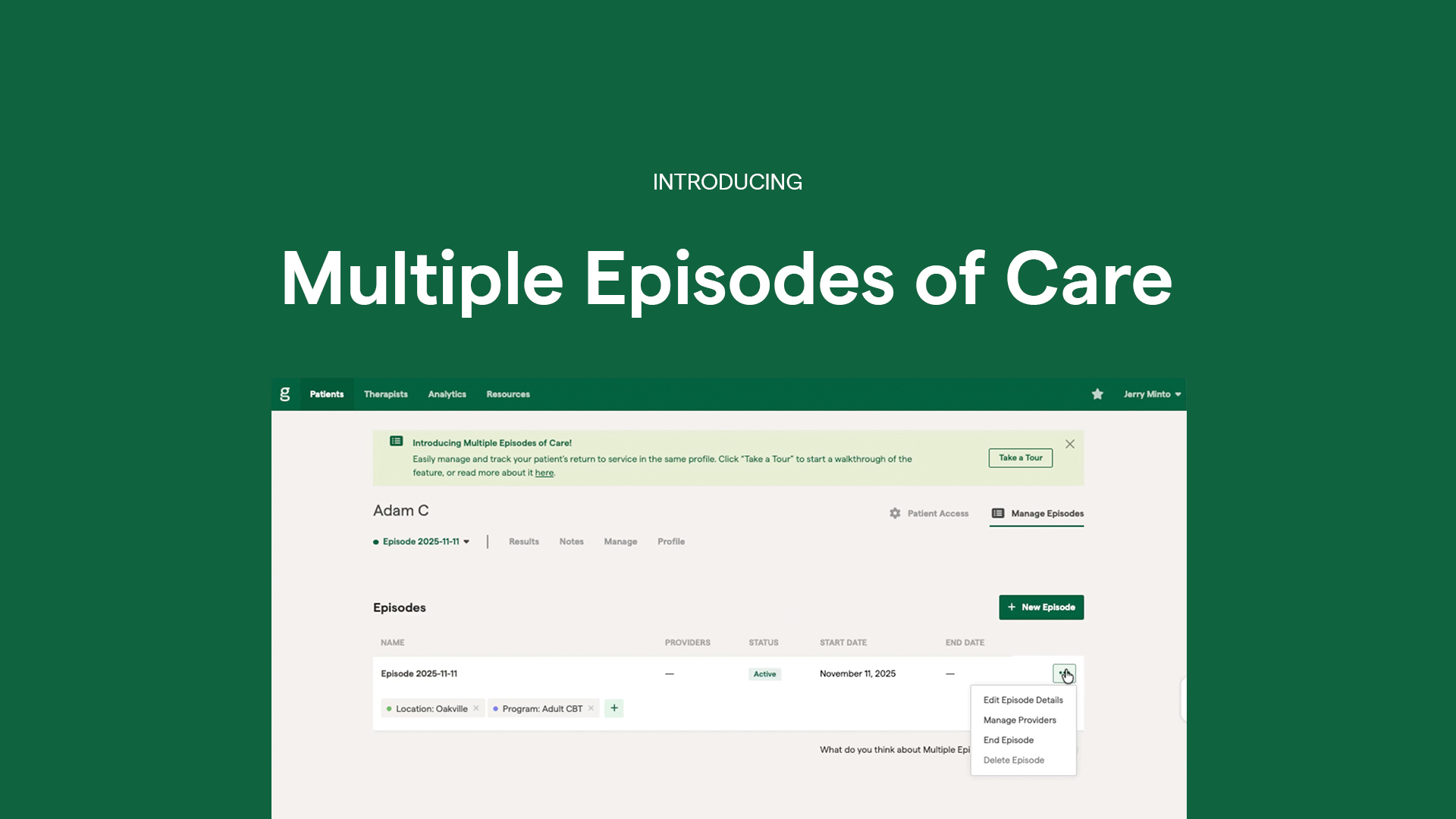
In 2024, Within Health partnered with Greenspace to implement Measurement-Based Care (MBC), integrating routine assessments across their care model to monitor client progress and strengthen clinical decision-making. Dr. Wendy Oliver-Pyatt, Co-Founder, CEO and Chief Medical Officer of Within Health, joined our recent educational webinar, ‘Enhancing Eating Disorder Treatment: The Value and Impact of Measurement-Based Care‘ to share their implementation journey and the impact of MBC on client care. Here’s what we learned.
Implementing Measurement-Based Care in Practice
Committed to using evidence-based practices to provide highly personalized, effective treatment experiences for their patients, Within incorporated standardized, validated patient-reported outcome measures (PROMs) into their treatment plans, using Greenspace’s MBC solution. At Within, PROMs are administered throughout treatment at three levels: at admission to determine baseline levels, monthly during treatment to measure progress and determine treatment efficacy, and at discharge.
1. Getting Started: Introducing MBC at Your Organization
Wendy is joined by an exceptional team of clinicians at Within Health, dedicated to improving the client experience and providing high-quality, eating disorder care. When implementing MBC, she emphasizes the importance of both the client and clinician being well-informed about the process and impact that it will have on improving treatment outcomes. Watch the clip below for advice from Wendy on introducing MBC to your team.
Prioritizing collaboration and education on the value of MBC helps providers understand the importance of incorporating outcome measures into the treatment process. From there, it’s important that leadership continues to emphasize the process, encourage clinical engagement, and demonstrate how the data is being used across the organization to innovate and improve care. Learn more about why MBC matters for providers and clients.
2. Getting Started: Supporting Clinicians and Staff Implementing MBC
Introducing MBC into the treatment process can be intimidating for clinicians and clients, who may not be well-informed about how to effectively introduce PROMs and use outcome data to guide treatment decisions. Some team members at Within initially felt unsure about how to administer measures accurately, interpret the results, or explain their purpose to patients. Questions also arose around ensuring data quality and using it meaningfully within therapeutic conversations.
To address these concerns, the team at Within has focused on education, collaboration, and practical tools to get a better understanding of MBC and gain confidence in implementing it effectively. Clinicians took the time to gain a deeper understanding of each measure, developed personalized ways to introduce them in sessions, and used resources like printed reports to support real-time conversations with clients. Regular team discussions helped connect data trends with clinical observations, building confidence in incorporating MBC as an integral part of client-centered care.
In this video, Wendy addresses and debunks common misconceptions around MBC.
3. Getting Started: Selecting Outcome Measures for Eating Disorder Treatment
Within uses 5 core PROMs for patients presenting with eating disorder symptoms: Eating Disorder Examination Questionnaire (EDE-Q), Clinical Impairment Assessment Questionnaire (CIA), Intuitive Eating Scale-2 (IES-2), Patient Health Questionnaire-9 (PHQ-9), and Generalized Anxiety Disorder (GAD-7).
In the following clip, Wendy discusses the outcome measures they use in eating disorder treatment, which follow guidelines from the Red Sea Coalition, and context as to why they have been selected for their programming.
For more information on outcome measures used in eating disorder treatment and guidance on selecting the best measures for your practice, visit this article.
4. MBC in Practice: Using Outcome Measures to Inform Eating Disorder Treatment
PROMs provide a way for clinicians and clients to routinely check in, review objective data on symptom changes, and identify insights or patterns that can serve as a guide for treatment adjustments or decisions. Clinicians can review ongoing progress measures to make evidence-based decisions regarding the course of treatment, while also observing the efficacy of current treatment plans to determine if they’re helping the client progress.
Watch the clip below, where Dr. Wendy Oliver Pyatt offers a client example to demonstrate how treatment plans at Within Health are adapted based on PROMs.
In this example, the measures provided an avenue for a collaborative conversation that helped the provider uncover helpful insight into the symptoms and experience of the client. This newfound information was important to understanding the complexities of the client’s experience, and in turn, the correct course of treatment.
In the next clip, Wendy shares a case where the PCL-5 assessment had an impact on a client, bringing self-awareness to their condition and invoking important conversations regarding treatment.
5. MBC In Practice: Monitoring Co-occurring Conditions and Discharge Readiness
Measurement-Based Care brings so much additional value to treatment, especially in eating disorder settings, where measures can empower providers to (a) monitor co-occurring conditions and (b) identify the end of treatment.
(a) It is common in eating disorder treatment for clients to present with one or more co-occurring conditions. Often times, the eating disorder is addressed as a priority, and the co-occurring condition is overlooked and left untreated. The use of PROMs enables providers to monitor these conditions throughout treatment, empowering them to reliably determine how these symptoms are actually affecting the patient and might impact the course of treatment.
(b) In the clip below, Wendy explains the importance of monitoring co-occurring conditions, as well as how PROMs influence higher treatment completion rates by reliably determining when patients are actually done with treatment, rather just when physical symptoms have disappeared.
Wendy’s example illustrates one of the key driving forces for implementing MBC throughout the treatment process. Physical, external indicators don’t tell the whole story; having the patient report their symptoms and feelings consistently will help providers track meaningful changes over time and assess when a patient is truly making progress towards recovery.
6. MBC in Practice: Transitioning Out of Care with MBC
Eating disorders are often battled even after treatment is done and the patient has recovered. At Within, Wendy believes in gradually transitioning clients out of care by incorporating exposure to things outside of treatment, and leveraging MBC to inform this process. PROMs can be incorporated to determine when clients are ready for a transition period, and whether they continue to progress with their recovery throughout this process.
Watch the clip below for more information on how clients at Within are gradually transitioned out of care with MBC.
Key Impacts of MBC in Eating Disorder Treatment at Within Health
MBC is integrated into various steps of the treatment process at Within, and has become an integral step in effectively supporting patients with high-quality, evidence-informed care. Here are a few of the ways that MBC has led to significant clinical improvements at Within that have enhanced operations and client outcomes:
1. Improved Clinical Decision-Making: Ongoing progress monitoring allows the clinicians at Within Health to tailor treatment in real time, make informed decisions about care adjustments, and ensure clients are receiving the right support based on their individual needs.
2. Strengthened Collaboration & Communication: MBC enhances communication between providers, clients, and families by providing objective outcome data that power collaborative discussions and elevate therapeutic alliance. Given the high rates of treatment resistance in eating disorder care, it is vital that the client is able to clearly communicate their needs and perspective throughout care. The measures offer an effective way to ground conversations between providers, clients, and their families, to ensure everyone is aligned on the goals of care and the best approach to meeting them.
3. Empowered Clients: Sharing outcome data with clients fosters transparency, encourages engagement, and often increases willingness to stay in treatment and actively participate in their recovery. Clients at Within report feeling supported and hopeful, with one client sharing:
“I have the tools, support, and awareness in order to sustain the work that I have been doing and hopefully to move closer to life without an eating disorder. Within helped me realize that everything is possible, that I am capable, and I deserve to practice self-compassion.”
4. Demonstrated Outcomes & Improved Funding Opportunities: Tracking and analyzing outcomes over time supports continuous quality improvement and helps Within communicate the impact of their services to external stakeholders, including payors and partners.
Wrapping Up
MBC has the power to transform eating disorder treatment, equipping clinicians with outcome data to make evidence-based decisions and empowering clients throughout their recovery. At Within Health, its thoughtful integration across the treatment journey has helped clinicians deliver more personalized, data-informed care, foster deeper collaboration with clients, and build stronger outcomes that last beyond discharge.
Their story is a powerful reminder that recovery is complex, and real progress goes beyond surface-level change. With the right tools and approach through MBC, we can elevate care and ensure that every individual receives the support they need to thrive.
Want to explore how MBC could strengthen your approach to care? Schedule a call with one of our implementation experts or reach out at info@greenspacehealth.com.