Article One: Transitioning to Remote Service Delivery
Mental health and wellness services have been forced to implement significant changes to service delivery in order to adapt to the COVID-19 pandemic. These organization have been faced with new challenges, including the need to drastically change traditional service delivery models, learning and implementing secure and confidential platforms for online mental health services, and providing support for staff in transitioning their practice to operate virtually.
We interviewed staff from four Canadian mental health agencies and private clinics to discuss experiences in adapting their organizations’ practices and services amidst the pandemic. Insights gathered from the discussions will be presented in four articles. This first highlights the practical aspects of how each organization quickly transitioned to offering remote services. The second article will explore changes in client engagement and clinician buy-in and how these challenges were addressed. The third article will break down the successes and challenges of remote-service delivery, and lastly, the final article will discuss the next steps for these services, and the lasting (or temporary) impacts these changes will have on their organizations.
The mental health organizations included in this series are:
- York Hills Centre for Children, Youth and Families
- Catholic Family Services of Toronto
- Queen Square Family Health Team
- DBT Hamilton
Prior to the pandemic, York Hills Centre for Children, Youth and Families were not offering any remote services. Clinical Director Simone Shindler said, “the agency had always wanted to expand services to offer more online options, however the busyness of day-to-day operations always got in the way.” COVID-19 served as the impetus for York Hills to quickly begin offering video counselling through Microsoft Teams and Zoom (business), both being secure, PHIPA compliant platforms. One key decision that the agency made was in making the commitment that clinical programs would still run during the pandemic, in order provide continuous care to clients during this difficult time. In order to support the staff through these changes, York Hills developed protocols and internal training for working remotely, including how to set up a confidential workspace, and how to conduct webinars and groups online. The agency was able to successfully transition their walk-in counselling program to a phone line called ‘Here 2 Help’ , which runs 3 days per week, providing single session therapy to callers looking for immediate support. Additionally, the day treatment classrooms were also conducted virtually to allow for a continuation of service to children and youth requiring this specialized support. Training was provided to support the clinical work, for example teleplay, which provided guidance in how to conduct play therapy remotely.
Similar to York Hills, Queen Square Family Health Team had no virtual care established prior to COVID-19. At the beginning of March, the team anticipated that the situation would escalate to a full lock-down, and changes would need to happen. During a team meeting, Clinical Program Manager Noreen Syed shared that clinicians were asked, “in the event this escalates to a full lock-down, could you see yourself operating in a virtual care model?” The majority of the team responded yes, many of whom already had experience using virtual care methods such as phone or video in their private practices. During the second week of March the team operationalized their transition to remote care by choosing Zoom as their PHIPA compliant video platform. All training for staff was done internally and led by team members with experience using Zoom in their private practice. Additionally, the admin team received training in supporting the clinicians and clients in setting up remote therapy. This proactive preparation resulted in no service delays when Queen Square was required to be fully remote due to the COVID-19 lock-down.
Catholic Family Services Toronto (CFS Toronto) made the decision to transition to remote service delivery in mid-March; by the last week of March they were fully transitioned. Prior to the pandemic, CFS Toronto had been using an online telehealth platform, but only with a small percentage of clients. Currently, the majority of the counsellors are offering a combination of phone and video counselling. To successfully transition all services, the agency engaged in informal training, led by staff members who were more tech savvy and experienced in providing remote services. Florence Loh, Manager of Programs and Services said, “for our clinicians who were less familiar with remote counselling, we encouraged them to first get used to the online counselling platform on their own, then try it with one client who was more tech-savvy. Then progress to using it with more clients with different levels of understanding in terms of technology. Learning the technology was done by trial and error”.
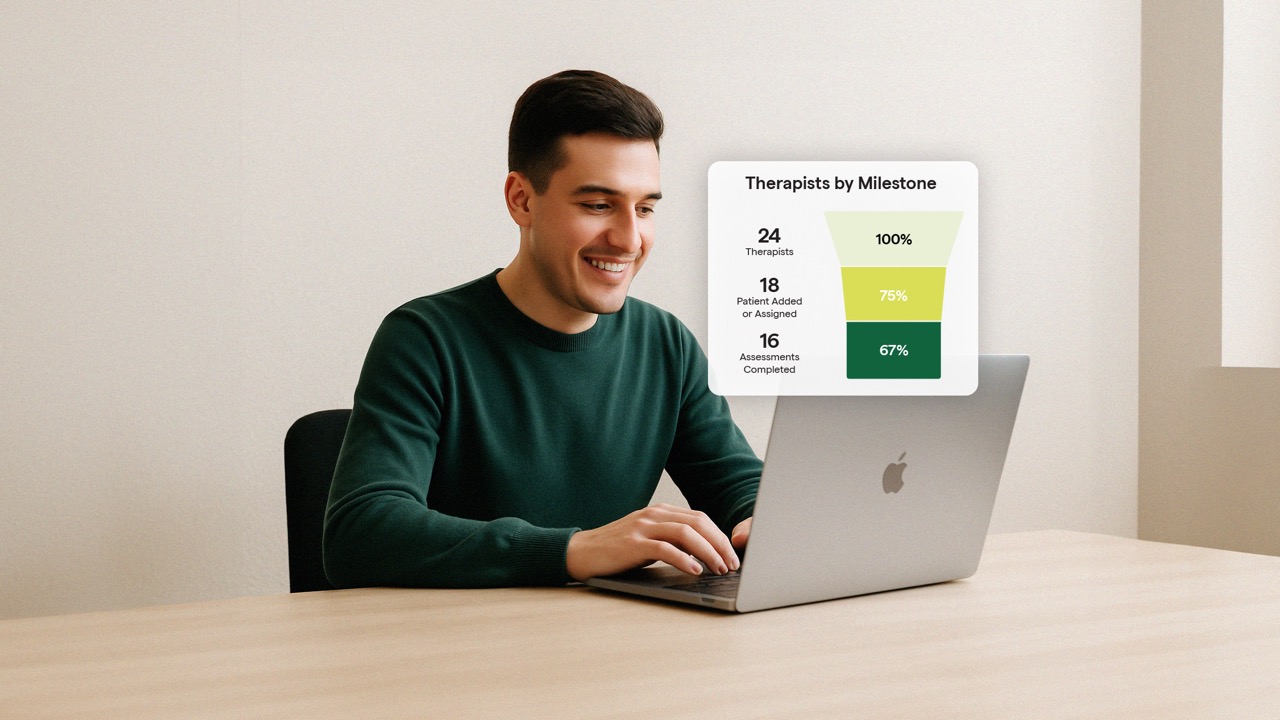
DBT Hamilton had been providing limited virtual sessions prior to COVID-19, only offering video counselling in special circumstances, for example during inclement weather or for individuals who lived very far away. The clinic implemented a three phased approach to be able to fully transition to remote service delivery. Phase one was to get all clinicians and clients setup with the software necessary to support virtual sessions. Phase two was to launch group therapy sessions remotely, which took exploration and critical thinking as to what would work best, as the Clinician’s predicted there may be some issues related to privacy and confidentiality. Lisa Burckell, the founder of the clinic shared that “some client’s felt comfortable with online group counselling however others did not feel comfortable having their face seen. The clients who were not comfortable with this interface were put on a waitlist for in-person services.” Phase three was to resume new assessments and transition all consent forms online. DBT Hamilton used Greenspace as a resource to onboard new clients, as it allowed them to deliver standardized assessments virtually.
Next…
Each of these organizations quickly adapted to the unique circumstances of the COVID-19 pandemic. The next article will explore how these services adjusted to changes in client engagement and clinician buy-in amidst the COVID-19 pandemic.